Nutritional Status of Subjects with Celiac Disease (CD) at a Tertiary Care Hospital in Saudi Arabia - A Retrospective Cross-Sectional Study by Kavita Sudersanadas in Open Access Journal of Biogeneric Science and Research
ABSTRACT
Introduction: Celiac disease (CD) is chronic gluten-sensitivity enteropathy. Due to the inflammatory reactions, it is known to cause malnutrition. Objective: The study aimed to assess the nutritional status of subjects with CD by anthropometric, biochemical methods.
Subjects and Methods: The study followed a retrospective cross-sectional design-seventy-one subjects with CD registered in a tertiary care teaching hospital from 2008 to 2018. Data concerning demography, clinical manifestations, and the biochemical and iron profile of the selected subjects were collected by using IRB-approved data collection form from the Best Care Hospital Information system. The data were analyzed by using SPSS Version 22. Categorical variables and continuous variables were expressed respectively by frequencies and percentages and by mean ± Comparison of mean values was done with student's t-test. The IRB of KAIMRC approved the study.
Results: The age of the subjects ranged from 3 to > 60 years. The majority (78.9%) of them were females. Moderate to severe underweight was found respectively among female and male children of 3-12 years. Adequate nutrition was reported among 13-18 years. According to BMI for age percentile, the prevalence of malnutrition among children was 8.7%, whereas 26.1% of the children with CD were either overweight or obese. BMI of adult subjects indicated that 29.6% were with energy deficiency and 32.4 % were overweight or obese. Iron deficiency was the most prevalent micronutrient deficiency found among the subjects, especially among females.
Conclusion: Those with CD are at risk of iron efficiency anemia and loss of lean mass. Loss of lean mass and severe undernutrition results in growth retardation. The study indicates the importance of nutrition monitoring and follow up and nutrient supplementation to those with CD.
KEYWORDS: Celiac disease; Nutritional status; Anthropometry; Biochemical profile; Iron profile
Introduction
Celiac disease, known as gluten-sensitivity enteropathy, is a chronic autoimmune inflammatory disease in the small intestine. It is characterized by permanent gluten intolerance and malabsorption syndrome. The etiology of CD could be due to environmental factors such as the ingestion of gluten and genetic factors such as HLA and tTG auto-antigen. Therefore, CD affects genetically susceptible individuals. Gluten is recognized as a protein found in prolamine fragments of barley (hordein), wheat (glutenin and gliadin), or rye (secalin) [1–5].
CD could be associated with autoimmune diseases such as diabetes, type 1, and hypothyroidism. Over the previous decades, the prevalence rate of celiac disease in different parts of the world was underestimated by relatively 1 in 1000 individuals. It was considered an uncommon disease that mainly affects children, and typical symptoms, gastrointestinal manifestations. The gastrointestinal manifestations are chronic diarrhea, vomiting, bloating, abdominal pain, abdominal distention, and steatorrhea. The recent introduction of susceptible serological tests led to increased screening. The subjects with CD are diagnosed by serological tests such as tTG, anti-gliadin, and EMA. They can be diagnosed by small intestinal mucosal biopsy, which is treated as the golden standard for CD diagnosis (5-11). Accordingly, the prevalence of CD is increased continuously at the rate of 1 in 100 or 200 individuals. High rates of prevalence were reported among females than males (2.8:1) [2,4, 12-14]. In KSA, it was reported that females have a high prevalence of CD than among males [12].
The CD is classified into typical (with gastrointestinal manifestations), atypical (extra-intestinal manifestations), and asymptomatic [1, 2, 14-16]. Extra-intestinal manifestations include fatigue, dermatitis herpetiform, and bone problems such as osteopenia, hematological abnormalities such as anemia; leukopenia; thrombocytopenia; and thrombocytosis.
The inflammatory reaction causes morphological changes in the proximal small intestine, which ate villous atrophy, abnormal surface epithelium, typical flat mucosa, and hyperplastic crypts. These morphological changes occur primarily in the duodenum and jejunum and because malabsorption leads to nutrient deficiencies [2, 4,13,14,17,18]. There is much evidence that the macronutrients and micronutrients deficiency among individuals with CD is higher than those without CD [4, 18]. Iron deficiency anemia (IDA) due to iron deficiency is the main hematological magnification found in subclinical cases of CD and could be the only manifestation observed with CD subjects. Iron deficiency can result from iron malabsorption, gastrointestinal bleeding, or iron loss via diarrhea or steatorrhea. IDA is usually considered as presenting feature of CD. 0.5%-6% cases of IDA result from CD.
Numerous studies documented the impact of nutrient malabsorption caused by CD in both children and adults. Although gluten sensitivity is temporary and resolves with the healing of the small intestine, additional restrictions to a gluten-free diet increase the risk of overall nutritional deficiencies. This study aimed to assess the nutritional status of subjects with CD as depicted by biochemical and iron profiles.
SUBJECTS AND METHODS
The study was conducted at the gastroenterology department of King Abdulaziz Medical City from 2008 to 2018. KAMC is one of the biggest hospitals in KSA located in Riyadh. It has 690 beds tertiary care, and it is a teaching hospital.
Subjects
All patients, irrespective of gender, registered in King Abdul-Aziz Medical City and referred to the gastroenterology department with a diagnosis of celiac disease were included in this retrospective cross sessional study. Exclusion criteria included those with pregnancy or lactating mothers, patients with apparent blood loss (not caused by celiac disease) such as hypermenorrhea, Melena, hemoptysis, those with gastrointestinal abnormalities such as irritable syndrome, chronic liver disease, chronic kidney disease, and Crohn's disease, those with febrile diseases such tuberculosis, those with cancer of intestine/ colon/ or any organ in the gastrointestinal tract and those who have metabolic disorders. Accordingly, 71 patients were selected for the study by using the convenience sampling technique.
Data Management and Analysis
Data were collected from the hospital information system, Best Care of KAMC. Data concerning demography, clinical manifestation, and biochemical and iron profile of the subjects were taken using IRB Approved Data collection charts.
The nutritional status of the subjects was assessed by anthropometric and variables related to the biochemical and iron profile. For children, Body Mass Index (BMI) for age percentile based on CDC growth chart was used to conclude anthropometric data. Those with less than the fifth percentile were considered underweight, 5- 85th percentile as normal BMI, 85 < 95th percentile as overweight, and equal to or ≥95th percentile as obese [19]. In addition, the subjects' weight and height were used to calculate BMI and classified as per universally accepted classification of BMI. The ideal body weight and percent of ideal body weight was calculated using MediCalc online calculator [20].
The collected data was entered in MS excel. After proper cleaning of the data, it was exported in SPSS version 20 for further statistical analysis. Prior to statistical analysis, the normality of the data was tested by Shapiro Wilk’s test. Categorical variables were presented by frequencies and percentages while for continuous variables mean ± SD was used. Mean values were compared by using an independent t-test. Statistical significance of the test was assumed with p-value of <0.05 [21].
RESULTS
A total of 71 subjects with confirmed celiac disease diagnosed by duodenum biopsy and serological tests were identified and included in the study. Table 1 details the demographic characteristics of the subjects.It was observed that the majority of the subjects were in the age group of 30-60 years (35.2%), followed by those in the age group of 18-29 years (29.6%) and more than ¾th of them (78.9%) were females. The important gastrointestinal manifestations reported were diarrhea (29.6%), abdominal pain (26.8%), and vomiting (25.5%). In addition, around 26.8% were diagnosed with extra-intestinal manifestations such as skin lesions.
Table 1: Demographic Characteristics of the Subjects with CD

*Some Subject Presented with More Than One Clinical Manifestation
The nutritional status of the subjects based on anthropometric data is given in Table 2. It was observed from Table 2 that there was significant gender variation in height, current body weight, and ideal body weight of the subjects of age 19-50years. In addition, the percent of ideal body weight (%IBW) was 21.4 and 24.3 respectively for adult females and males, and there is a significant gender difference in % of IBW. A significant difference in IBW was observed among females and males of 13-18year old subjects. Severe underweight observed among the subjects of age group 2-12years and 19-50years. CD is one of the etiological factors for malnutrition among adults and children.
Table 2: Nutritional status of the subjects as depicted by anthropometry
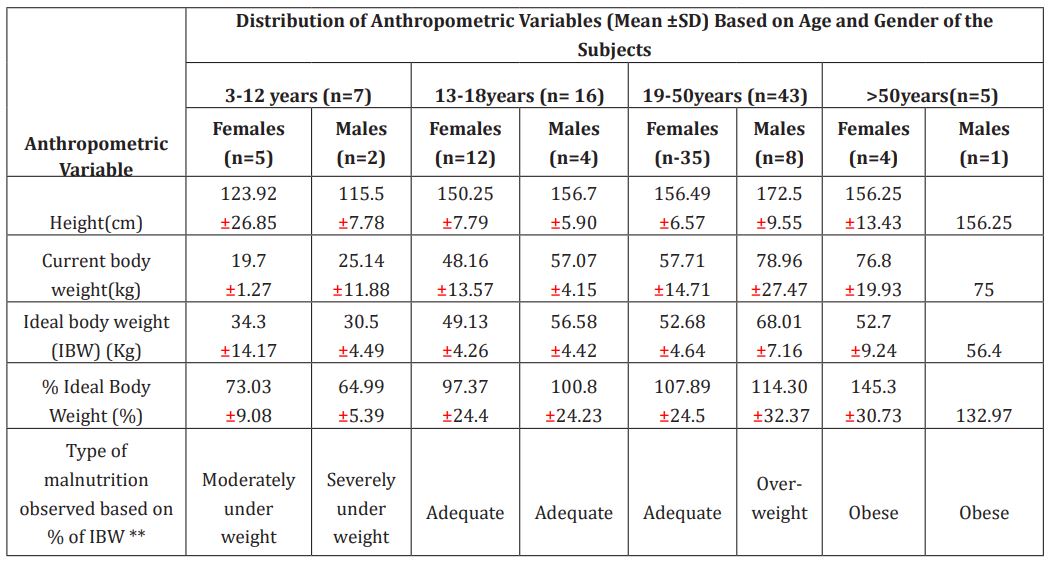
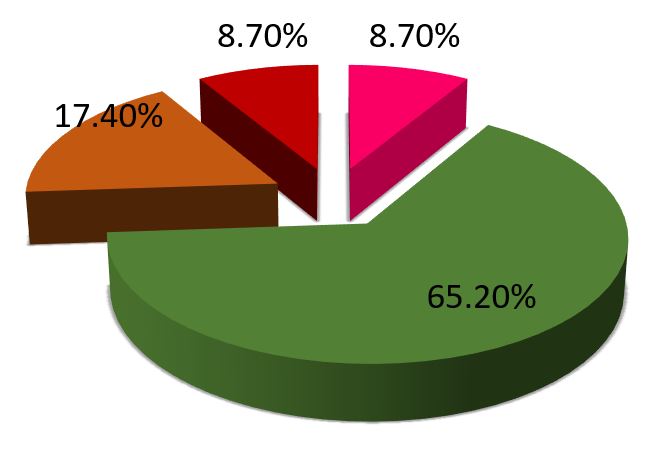
Prevalence of energy deficiency among the subjects as indicated by Body Mass Index is given in Figure 1 and 2.
It was found that the prevalence of energy deficiency as indicated by Body Mass Index (BMI) ranges among children aged 2-19 years old with CD was 8.7%. Most child subjects (65.2%) had normal BMI; however, 17.4% were overweight, and 8.7% were obese. Among the adults, 29.6 percent had energy deficiency, whereas 38 % were of normal BMI (Figure 2). The biochemical profile of the subjects with CD is given in Table 3. The biochemical profile of the subjects indicated that compared to males, female subjects are at risk of low biochemical values. The majority (25%) of the subjects were presented with lower blood urea and serum creatinine (25.35%). In addition, there was a significant difference between blood urea and serum creatinine values of females and males. Table 4 details the iron profile of subjects with Celiac Disease. Results of the study indicated that compared to male subjects, female subjects are at greater risk of iron deficiency. Around 41.07 % of females presented low hemoglobin levels (Table 4). A significant difference existed between the hemoglobin values of male and female subjects (p= 0.001). The majority (73.21%) of the female subjects showed low serum iron levels. Low serum ferritin levels were found among 33.33% of males and 19.64 % of females. There was a significant difference (p= 0.012) between the serum ferritin values among both genders. Females with high total iron-binding capacity were at a higher percentage (78.57%) than males with CD (73.33%).
Table 3: Biochemical profile of the subjects with Celiac Disease
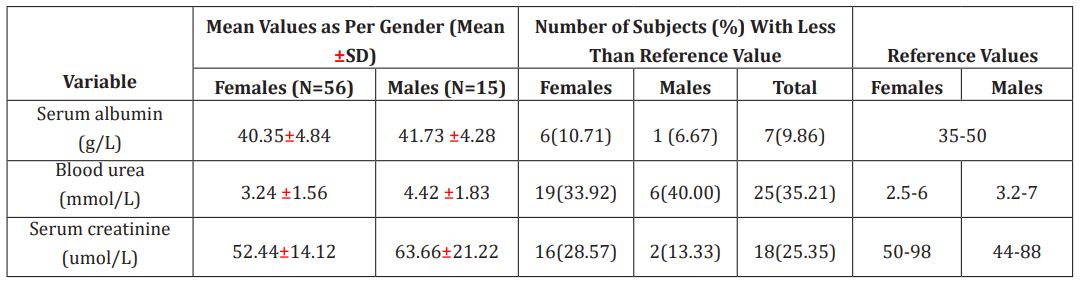
Figure 1 : Energy deficiency among subjects of 3-18 years as per BMI for age percentile
Figure 2: Energy deficiency among subjects of >18 years as per BMI
Table 4: Iron profile of the subjects with Celiac Disease

DISCUSSION AND CONCLUSION
Celiac disease (CD) is a chronic autoimmune inflammatory disease. In the present study, adults formed a significant proportion of the sample (64.8%), followed by 31% of children. Gender-wise distribution of the study subjects showed that females (78.9%) were more affected with CD. In addition, meta-analysis studies based on the seropositive diagnosis of CD from KSA showed that seropositive females are more common than males [22].
CD causes morphological changes in the duodenum and jejunum, which are the main sites of nutrient absorption. Gastrointestinal manifestations such as diarrhea (29.6%), abdominal pain (26.8%), and vomiting (25.4%) were reported by the subjects of the current study. These clinical manifestations interfere with the digestion and absorption of food and nutrients, resulting in nutritional deficiencies. Many studies support the evidence that, the macronutrient and micronutrient deficiency among individuals with CD is higher than those without CD [4,10]. The main finding of our study showed that the subjects experienced malnutrition due to chronic energy and iron deficiency.
Based on %IBW, children of 3-12 years of age were more affected with malnutrition than other age groups. They were categorized as moderate (females) to severely (males) underweight. Other age groups under the study were with good, overweight, and obese category of %IBW.
BMI for age percentile of the children was low for 8.7%. On the contrary, in a retrospective study conducted in Iran, the prevalence of malnutrition among child subjects with CD was 43% [23]. BMI of those above 18 years indicated that most (32.4%) of them were obese or overweight, whereas 29.6% were underweight. It was reported that overweight and obesity could co-exist with CD [24].
The loss of villi and surface epithelium due to CD increases the plasma protein leakage in such patients [25]. About 9.86 percent of the subjects of the study were presented with low serum albumin levels indicative of protein-losing enteropathy. Moreover, 35.21 % of the subjects had low serum urea, representing protein malnutrition or a low protein diet. Low muscle mass due to malnutrition is the leading cause of low creatinine levels. In the present study, 25.35% of the subjects were with low serum creatinine values. Iron is the major micronutrient depleted in subjects with CD caused by iron malabsorption, reduced duodenal iron absorption, gastrointestinal blood loss, autoimmune diseases, and microcytic anemia. The frequency of Iron Deficiency Anemia (IDA) among those with CD ranged from 12% to 69% [25]. This study found that 38.03% of subjects had low hemoglobin levels, and 67.61 % had low serum iron levels. Low serum ferritin, the marker of iron stores in the body, was observed among 22.54% of the subjects. It was stated that the depletion in body iron storage and reduced hemoglobin levels were observed among patients with celiac disease [26].
With the reduction in the body iron stores, there will be an elevation in the iron-binding capacity of the iron transporting protein transferrin. We found that 77.46 percent of the study subjects had elevated Total Iron binding Capacity (TIBC). In addition, females with CD are at higher risk for iron depletion in the body than males.
The strength of our study is that, it is the first study in KSA which indicates the nutritional status of subjects with CD by anthropometric, biochemical and iron profile for all ages. However, this study had certain limitations. The design of the study was retrospective. The samples with incomplete file records were excluded; hence the sample size was drastically reduced, and the sample size was very low for specific age and gender groups.
Celiac disease is chronic gluten-sensitivity enteropathy with varying clinical manifestations. Due to the inflammatory reactions and morphological changes at the micro and macronutrient absorption sites, the patients are at risk of nutrient deficiencies. Furthermore, nutrition and food consumption pattern in Saudi Arabia largely depends on cereal groups, with wheat as the most popular staple food. Therefore, improper nutritional management of CD may result in an unchanged or increased risk of having complications due to multiple nutrient deficiencies. In this regard, the changes in biochemical and iron profile due to iron depletion require more attention and follow-up. In addition, the results of our study indicated the importance of nutritional and lab assessments, Gluten-Free Diet, diet counseling, iron supplementation, and continuous follow-up and monitoring of the interventions with CD subjects during nutrition rehabilitation.
More information regarding this Article visit: OAJBGSR
https://biogenericpublishers.com/pdf/JBGSR.MS.ID.00243.pdf
https://biogenericpublishers.com/jbgsr-ms-id-00243-text/


No comments:
Post a Comment