Citrus Melanose and Quality Degradation of Fruit by this Disease: A Review by Fazal ur Rehman* in Open Access Journal of Biogeneric Science and Research (JBGSR)
Abstract
Citrus melanose, caused by Diaporthe citri Wolf, is a worldwide fungal disease that is prevalent in many citrus growing areas of Pakistan as well as in the world. Out of two stages of Diaporthe citri Wolf i.e. perfect stage and imperfect stage, the perfect stage causes the citrus melanose disease in many citrus species. Extended rainfall with warm environmental conditions favours the disease initiation and development. This disease result in degradation of fruit quality that results in reduction of marketing and export values of fruit. Proper pruning and use of copper based fungicides are advisable for the treatment of citrus melanose. Plantation of susceptible varieties should be avoided in high rainfall areas. In this article, history of citrus melanose, symptoms of disease, pathogen, epidemiology of disease, quality degradation of fruit and integrated management practices has been discused.
Keywords: Diaporthe citri Wolf; Mud cake Melanose: Teleomorph; Anamorph; Copper-based fungicides
History of Citrus Melanose
The perfect and imperfect stages of Diaporthe citri Wolf cause two different citrus diseases with perfect stage causing citrus Melanose and imperfect stage causing Phomopsis stem-end rot Swingle and Webber firstly described citrus melanose disease near Citra, Floridain 1892 [1]. In 1912, Floyd and Stevens published with evidences that stem-end rot and melanose were caused by the same fungus. At that time they were unable to produce the isolates of fungus from the infected leaves showing the symptoms of citrus melanose on inoculation. The comparison of P.citri and D.citri was made by Fawcetin1932 [2].
In 1940, Ruchle and Kuntz demonstrated that the spores of both P.citri and D.citri had anability to cause the symptoms of citrus melanose [3].Initialy, D.citri was given the name of D.melusaea. But on later, D.citri was given the priority over D.melusaea by Fisher in1972 [3].P.cytosporela was also used for P.citri and it was also proposed that P.cytosporella should be used in place of P.citri. But this proposal was never adopted. The genus Diaporthe/ Phemopsis was place dinphylum Ascomycota with class and order as Sordariomycetes and Diaporthales respectively [4][5]. Four species were found to be different from F.valgure based on their molecular, morphological and cultural data [6]. According to the studies of Gome they have a wide range of host and have ability to form colony on the host that may be diseased plant or dead plant [7]. It was recognized as them most actively transmitting pathogen of citrus.
Symptoms of the Disease
The citrus melanose disease, which is superficial and has no effects on internal quality of fruit but cause the external quality degradation, produces its symptoms on fruits, leaves and small twigs. In case of foliage, the symptoms appear with the formation of small water-soaked speaks that on later become centrally depressed and surrounded by undepressed translucent yellow arcas [8]. After a week, the exudation of gummy substances occurs due to the rapture of leaf cuticle that on later become brown in colour and hardened. These areas have sandpaper- like texture. In case of severe infection, the leaves become pale green to yelow.
The infections may occur on the green twigs .In case of severe infection, the defoliation Occurs that induces the twigs dieback [9].On fruit, scattered speaks are formed in case of high infestation. The infection on young fruits may causet the premature abscission of fruit. In case of late infection, flater pustules are produced. In severe cases, firstly the formation of solid patches of blemish and then cracking of fruit surface occurs, this condition is called mud cake melanose [10]. On the fruit surface, there is also formation of tear-streaks and water droplets patern. The formation of star melanose occurs by the late application of copper based fungicides on the diseased portion of plant because of formation of dark and corky lesions, more prominent then normal and are in star shape [11].
Pictorial Description of Symptoms: (Figures 1 & 2)
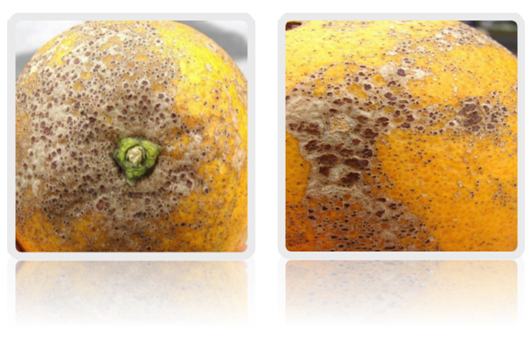
Figure1: Symptomatic lesions of Citrus Melanose present on fruit surface.

Figure 2: Lesions on leaf surface and formation of Star Melanose symptom on leaf.
Pathogen
The Teleomorph of fungal pathogen is Diaporthe citri Wolf and anamorph is Phomopsis citri Fawc. Mostly leaves and fruits are infected by Diaporthe citri Wolfand Phemopsis citri attacks on stem and causes the stem-end rot [11]. In citrus, fungal pathogen also acts as saprophyte for the infestation on dead twigs. The hyline ascospores of Diaporthe citri produced in each cell are slightly constructed at septum and are in the form of oil droplets. Ascospores are produced in flask shape perithecium. The average size of ascospores is 12.85 microns by 3.85 microns with the perithecium size on average is 500 microns by 50 microns at beak and the base is of diameter125to160microns[12].
The perithecium are projected outward from the stem. The ascospores are ejected from the perithecium forcefully and then they become air borne and spread out over the large distance [1]. On culture media, fan-shaped, white colored mycelia are produced [13]. When spores get substrates, they produce septate hyphae [12]. In disease cycle, the most important state of fungal pathogen is its conidial state. Two types of conidia i.e. alpha conidia and beta conidia are produced by the pathogen. The primary source of spread of fungal pathogen and with the size range from 5-9 microns by 2.5-4 microns are alpha conidia tha are hyaline and single celled. The beta conidia that are slender-rod shaped and hook-like at the end, are spread with great efficiency during rainy condition over nearby substrate and from mycelium [12].
Epidemiology of Disease
The attack of fungal pathogen causing citrus melanose is during the immature stage of foliage, fruits and twigs. Because when the tissues are matured, they mostly become more resistant to the attack of pathogen. Therefore, the susceptibility period for the attack of pathogen over the plant is the period of first 8 to9 weeks after their formation. The formation of symptoms of melanose can vary according to the level and the time of infection. The flyspeck melanose symptoms are produced at the end stage of susceptibility period [14].
As the discharge of ascospores is forcefully and they can be dispersed over the long distance, therefore, the inoculums of fungal pathogen can be spread over the large distance. That's why, there is an increase in the cases of infection be cause of wide spread of large number of ascospores [15]. The disease wil be initiated when the ascospores or conidia of Diaporthe stage or Phemopsis stage land on the surface of plant tisue. The favourable environmental conditions for the infection include dry conditions and the temperature ranging between 17 to 35°C. Above or below this temperature the spores mostly die and the chances of infection reduced [16].
About 10 to 24 hours of moisture are required for the germination of spores but approximately 36 to 48 hours are required for the germination as well as the formation of germ tube that directly penetrates into the tissue of cuticle layer [16]. Then the infection of citrus Melanose pathogen starts.
Quality Degradation of Fruit
Melanose is a serious disease of citrus plant which results in small spots on the surface of citrus fruit. These spots increase in number as the disease reaches its serious stage. These spots cover the entire surface of fruit and reduce the aesthetic quality of fruit. When the disease affects the young fruit, they remain small in size and fall of before reaching maturation stage. In this way, it also results in quality reduction. Atadvanced stage of disease, the spots produced are more solid and the surface of fruit becomes cracked. The fruit affected by melanose disease is not preferable for marketing and export purpose due to quality degradation and thus the market value and export of citrus reduced because the quality of citrus fruit is reduced. However, the disease does not affect the pulp so the fruit for processing purpose is not generally affected but the marketing and export of the diseased fruit is reduced due to the quality degradation and this may cause serious economic losses.
Melanose is a severe disease of citrus in most citrus producing countries and mostly the grape fruit and lemon are affected by this disease [17]. The quality and value of disease afected fruit is reduced and it is not accepted by consumers as a fresh fruit and marketing value is also reduced. The diseased fruit is used as low grade fruit for processing purposes. Farmers and exporters are economically affected due to value loss of citrus fruit by melanose disease.
Integrated management practices
Although, there is no any impact of disease over the yield, so the juice and processing also Remains unaffected But the quality of the fruit for marketing and export purpose is adversely afected. So following integrated management practices should be done for the control of quality losses and fruit degradation by citrus melanose.
a. Dead branches should be prune out periodicaly. The pruning will help to increase the circulation of air through canopy of plant to keep it dry and the sites for the survival of saprophytic pathogen will also be reduced. It will also enhance the effective penetration of fungicides through for foliage [18].
b. The fungicides should also be applied for the the disease control. Mostly the application of Copper-based fungicides is done worldwide. The symptoms of star melanose can also be produced over the application of Copper-based fungicides that are not the actual symptoms of this disease [19].
c. The plantation of susceptible varieties including sweet orange, grape fruit and pomelo should be avoided in high rainfall areas [20].
d. Other management practices should be done including plantation of citrus in low rainfall and sunny areas, proper sanitation should be done, and intercropping should be avoided.
Conclusion
The symptoms, signs, signals of fever are only seen at the presence of fever. During cancer, the symptom, signs, and signals of cancer are shown every time. A patient having cancer and fever at the same time, symptoms, signs, and signals of both cancer and fever are shown every time. A symptom of cancer never becomes a symptom of fever or a symptom of fever can never become a symptom of cancer.
If fever is a symptom, one symptom has no ability to make other symptoms
Fever makes numerous symptoms, signals, and actions, etc.
If fever is a symptom we cannot call a person as a fever patient
If fever is a symptom no treatment is required to reduce fever. Treatment is required only for disease and its cause. Our immune system never increase elevated the symptom in the hypothalamus.
To know more about our Journal click on https://biogenericpublishers.com/
Open Access Journal of Biogeneric Science and Research (OAJBGSR)
