Influence of Clinical Pathway Implementation on the Outcome of Drug Rehabilitation Program Services by Jaya Mualimin in Open Access Journal of Biogeneric Science and Research
Abstract
Patient safety, quality, and efficiency are global issues, therefore hospitals must be able to apply clinical pathways through clinical pathways as the main facilities and infrastructure, especially in services for increasingly acute drug addicts. This study aims to analyze the implementation of clinical pathways for drug rehabilitation program outcomes on 1) clinical quality, 2) cost, 3) readmission, 4) satisfaction, and 5) LOS, at RSJD Atma Husada Mahakam. This type of research uses cross-sectional with observational analytic, data collection through distributing questionnaires to 111 respondents, observation and literature study. The results showed that the clinical quality before and after the implementation of the clinical pathway had a significant effect, but the cost of treatment did not show any significance. There is a positive relationship between readmission and the implementation of clinical pathways, as well as addict satisfaction in the LOS rehabilitation room has a significant effect on treatment time and clinical pathways. A recommendation that the 5 (five) variables mentioned above, apart from being cost-effective, can improve the quality of drug rehabilitation services at RSJD Atma Husada Mahakam Samarinda, so it needs to be maintained
Keywords: Outcome; Quality Clinic; Readmission; Cost, Satisfaction; Length of Stay
Introduction
Drug dependence is a type of chronic recurrent brain disease and must receive therapy and rehabilitation. According to a 2016 BNN survey, the prevalence of drug abuse in East Kalimantan is 3.1% of the population aged 15-49 years. 10% of abusers experiencing health problems need to get medical help. Relapse will affect the quality, quality and patient safety (patient safety). if no preventive measures are taken with organizational policies. The cause of the high number of repeat patients/readmissions is uncontrolled relapse. One indicator of the quality and performance of the RSJD is to reduce the readmission rate, in 2015 the RSJD reduced the readmission rate to only 0.37%. [1].
The hospital implements quality management strategies such as total quality management, quality assurance, and continuous quality management. This strategy tends to focus on management aspects. The following professional aspects will review the definition. Clinical pathway (CP) is an integrated service planning concept that summarizes every step given to patients according to medical service standards, nursing care and other evidence-based services with measurable results. Several researchers have proven the implementation of clinical pathways. Implementation of clinical pathways in opiate therapy patients with methadone, can reduce the cost of therapy and the complications that arise are well controlled. concluded that the implementation of clinical pathways in the therapy of alcoholics, although not related to the length of stay (LOS) but was strongly related to outcome.
Devapriam et al., [2]: implementation of clinical pathways can increase the capacity of per-unit services, shorten the length of stay (LOS), increase the frequency of unit visits, timely assessment of care, and reduce variability in quality. concluded that the implementation of clinical pathways can calculate all types of guarantees or financing for each episode of treatment. Barbieri found significant results in the implementation of clinical pathways for care with a structured organizational approach (clinical governance) from the aspect of quality and low-cost service processes. Cheah said that the implementation of clinical pathways significantly reduces the treatment period and without any side effects or good outcomes. Susi Research, 2009; Chan and Wong, 1999; proves that clinical pathways are associated with increasing cost-effectiveness and significantly reducing the length of treatment.
Several other researchers have found evidence that treatment in one form of regulation (similar to a clinical pathway) can prevent relapse. Prince [3] and Marchisio,proved that making a scheduled treatment similar to a clinical pathway can be used as an indicator of reducing the three-month relapse rate. Before the intervention, the mean of relapse in the intervention group was 30.38% and the control group was 27.54%. After the intervention, there was a 20% reduction in relapse. In the schizophrenic group, 24% had an intervention, while 64% had no intervention [4-10].
Enforcement of clinical pathways for drug dependence Clinical pathways on drug dependence have not been widely studied so that research needs to be done. The implementation of clinical pathways that have been applied, can affect the outcome [11-15]. This study aims to analyze the effect of clinical pathway implementation on service outcomes in the drug rehabilitation program at RSJD Atma Husada Mahakam. The results of the study can be used as an evaluation of the clinical pathway implementation process for the inpatient drug rehabilitation program at RSJD Atma Husada Mahakam. The focus of the research relates to what is in the following picture (Figure 1).
Figure 1: Model Hypothesis
Method
This research method uses a survey model with a quantitative approach that focuses on 111 respondents (patients) who follow an inpatient drug rehabilitation program at Atma Husada Hospital (RSJAH) Mahakam, East Kalimantan, Indonesia [16-18]. The type of data is cross-sectional with analytical observation and literature review. Primary data was obtained from data from clinical pathway forms taken from addicts' medical records and reports on costs for services in drug rehabilitation programs [19-25]. The data analysis technique used the reliability and validity test of the instrument through the SPSS version 22 program, with the data analysis technique in the form of multiple linear regression and associative-causal. This is intended to be able to determine the relationship of influence between the independent variable and the dependent variable through partial and simultaneous tests and prove whether the alternative hypothesis (Ha) is accepted or rejected [25-30].
Research Result
Descriptive Analysis
Based on the results of the study, it was obtained that the description of the status of new patients was still greater than that of old or repeat patients. In (Table 1) in 2015 new patients were 84 addicts (75.7%) and in 2016 new patients were 102 addicts (89.5%). According to the 2016 BNN survey, the prevalence of drug abuse in East Kalimantan is 3.1% of the population aged 15 - 49 years. 10% of abusers experiencing health problems need to get medical help BNN, The prevalence rate of ever used decreased from 8.1% in 2006 to 3.8% in 2016. With the 2012 Accreditation plenary category, the Atma Husada Hospital has an impact on the stigma of mental illness and narcotics [31-35].
Table 1: Distribution of Respondents Characteristics.
Gender of respondents 84.8% are male. The results of this study according to the theory that there are more addicts in men than women, men are more at risk of using drugs than women. The ratio of men to women is about 4 to 1, meaning that among 4 male users there is 1 woman who has tried [36]. The prevalence rate was 13.7% for men and 3.3% for women (2006), while in 2016 it was 6.4% for men and 1.6% for women. The prevalence rate of ever tried using men tends to decrease from 13.7% (2006) to 6.4% (2016). However, in the female group, the trend of decreasing prevalence rates forever and a year using drugs began to be seen from 2009 to 2016 (BNN Survey, 2016).
According to data from the US Substance Abuse and Mental Health Services Administration in 2013, men are more dominant than women in substance abuse of all types and men often overdose and die than women. Including abuse of doctor's prescription. For most age groups, men have a higher level of dependence. However, women can also experience dependence. If women are dependent, the risk is stronger. Robbins et al 1999; Hitschfeld et al 2015; Fox et al 2014; Kennedy et al 2013 and more severe relapses, including women experiencing many legal and social complications including asocial behaviour and abuse. sexual. This problem causes the prevalence of women to be smaller than men [37-45].
Meanwhile, based on age group, table 4.3 was found in 2016 the most age groups were 17-25 late teens group of 115 patients (51.1%) and 26-35 years of early adulthood, 68 patients (30.2%). In 2015, the age group of 17-25 late teens was 58 patients (52.3%). In 2016 at the age of 17-25 late teens as many as 57 patients (50.0%), looking at this number it can be concluded that drug dependence users are dominated by the age group of late teens and early adults. Meanwhile, the education level of most drug rehabilitation patients is junior high school and senior high school, namely 175 (77.7%). In 2015, 2016 consecutively were 80 patients (72.0%), 95 patients (83.3%). However, the large proportion of drug abusers with a bachelor's degree in education does not mean they graduated, some of them are no longer in the campus environment, but are already working in various sectors or even some of them may be unemployed [46-50].
Meanwhile, judging from marital and unmarried status, the most addicted respondents were unmarried status with 121 (53.8%); 56.1% in 2016 and 51.3% in 2015. The place where addicts live is still the most in Samarinda City in 2015 there were 87 patients (78.4%) and in 2016 there were 48 patients (42.1%). In 2016 after the mandatory reporting program (IPWL) and the rehabilitation program for 100,000 addicts, the city of Balikpapan had 19 addicts, as can be seen in Table 1 below
Inferential Descriptive Analysis
LOS Drug Rehabilitation Patient
The average value for the length of stay for drug patients in 2015 or before the implementation of the clinical pathway, which was 42.29 days and in 2016 or after the implementation of the clinical pathway, which was 43.41 days, wherein 2015 it was 74 (66.7%). Meanwhile, in 2016 there were 65 (57.0) less or equal to the average value. The results of the independent sample t-test for LOS obtained p-value = 0.022 < 0.05, which means that there is a significant effect between LOS in 2015 (before clinical pathway implementation) and 2016 (before clinical pathway implementation).
Rehabilitation Patient Fee
The average cost in 2015 was Rp. 14,550,357.87 and in 2016 of Rp. 14,525,219.48, where the number of paying patients is below the mean value of 138 (61.3%). Regulation of the Minister of Health of the Republic of Indonesia. number 50 of 2016 that the cost of drug rehabilitation for a 1-month package is Rp. 6,500,000,000.00. When compared, the Ministry of Health tariff is much lower, if converted to days the Ministry of Health tariff is Rp. 216,666,-/day. the results of the independent sample t-test for the cost of care obtained a value of p = 0.98 > 0.05, which means that there is no significant effect between the cost of care in 2015 (before the implementation of the clinical pathway) and 2016 (before the implementation of the clinical pathway).
Service Quality
There are still a lot of new patient data from old or repeat patients. In 2015 new patients were 84 addicts (75.7%) and in 2016 new patients were 102 addicts (89.5%). From the repeat visit data in 2015 data, addicts who were readmission 2 times were 27 addicts (34.3%) while in 2016; addicts who were treated >2 times there were 12 addicts (10.9%). The results of the independent sample t-test for readmission obtained p-value = 0.006 < 0.05, which means that there is a significant effect between readmission in 2015 (before the implementation of clinical pathways) and 2016 (before the implementation of clinical pathways). Based on the results of the independent sample t-test of the clinical quality variable, the p-value = 0.042, the exit method p = 009 and the visit status p = 006 of the three variables, the p-value = < 0.05, which means a significant influence between clinical quality in 2015 (before implementation of clinical pathways) and 2016 (before the implementation of clinical pathways) [51-57].
Consumer Satisfaction
The satisfaction index of addicts who are being treated in the rehabilitation room is an average of 78.0%. All respondents' satisfaction variables gave satisfying answers above 93.3% to the implementation of clinical pathways asked respondents. The inferential statistics of the findings can be tabulated as follows (Table 2):
Table 2: Bivariate Analysis.
Discussion
With law no. 35 of 2009 on Narcotics article 54 that addicts must be rehabilitated medical and social rehabilitation, with PP no. 25 of 2011 concerning mandatory reporting for drug addicts, following the mandate of the narcotics law that mandatory reporting is the rehabilitation process for addicts at a mandatory reporting institution appointed by the ministry of health and social affairs. Although the diagnosis of drug dependence is included in ICD IX, it is not included in the BPJS health financing, so the government through this mandatory reporting program uses separate financing through the IPWL program. The regulation of the Minister of Health has been revised 3 times (Permenkes No. 50 of 2015) regarding the mandatory reporting technical guidelines for addicts and the procedures for financing and billing inpatient and outpatient rehabilitation costs for addicts.
The purpose of the clinical pathway is an efficient and effective rehabilitation process, reducing variations in procedures and reducing costs. Although cost savings are important, the use of clinical pathways must be evaluated, because the main focus is quality and patient safety. Van Herck et al., 82.5% of the studies reported a positive impact on cost reduction, while 13.5% did not explain the effect and 4% a negative effect.. A 2013 study on the introduction of clinical pathways in postoperative clinical care after major head and neck surgery found a 27% reduction in per-patient costs and several other studies have identified a reduction in length of stay after. Several researchers have proven the implementation of clinical pathways. Ronny Rivani (2014); Implementation of clinical pathways in opiate therapy patients with methadone, can reduce the cost of therapy and the complications that arise are well controlled.
Lacko et. al (2008): concluded that the implementation of clinical pathways can calculate all types of guarantees or financing for each episode of treatment. Barbieri (2009): found significant results in the implementation of clinical pathways for care with a structured organizational approach (clinical governance) from the aspect of quality and low-cost service processes. Cheah (2005): said that the implementation of clinical pathways significantly reduces the treatment period and without any side effects or good outcomes.
The use of clinical pathways has been associated with reduced hospital complications (Rotter et al., 2010) and improved service quality. Van Herck et al. found that 65.5% of the studies reported a positive effect on the outcome, while 32% reported no association with outcome. (Van Herck et al., 2000). Dowdeswell and Yasbeck cited previous studies providing quality and outcome for geriatric patients with depression, (Hindle, Dowdeswell and Yasbeck, 2004). According to Nielsen and Nielsen (2015) that the implementation of clinical pathways in the therapy of alcoholics, although is not related to the length of stay (LOS) but is closely related to the outcome.
The Avalos standard is based on the Minister of Health Regulation No. 50 of 2015 that the 1 monthly package for inpatient rehabilitation treatment is a minimum of 30 days. The average value for the length of stay for drug patients at the Atma Husada Mahakam Mental Hospital in 2015 or before the implementation of the clinical pathway was 42.29 days and in 2016 or after the implementation of the clinical pathway was 43.41 days, wherein 2015 there were 74 (66.7%) while in 2015 2016 as many as 65 (57.0) less or equal to the average value.
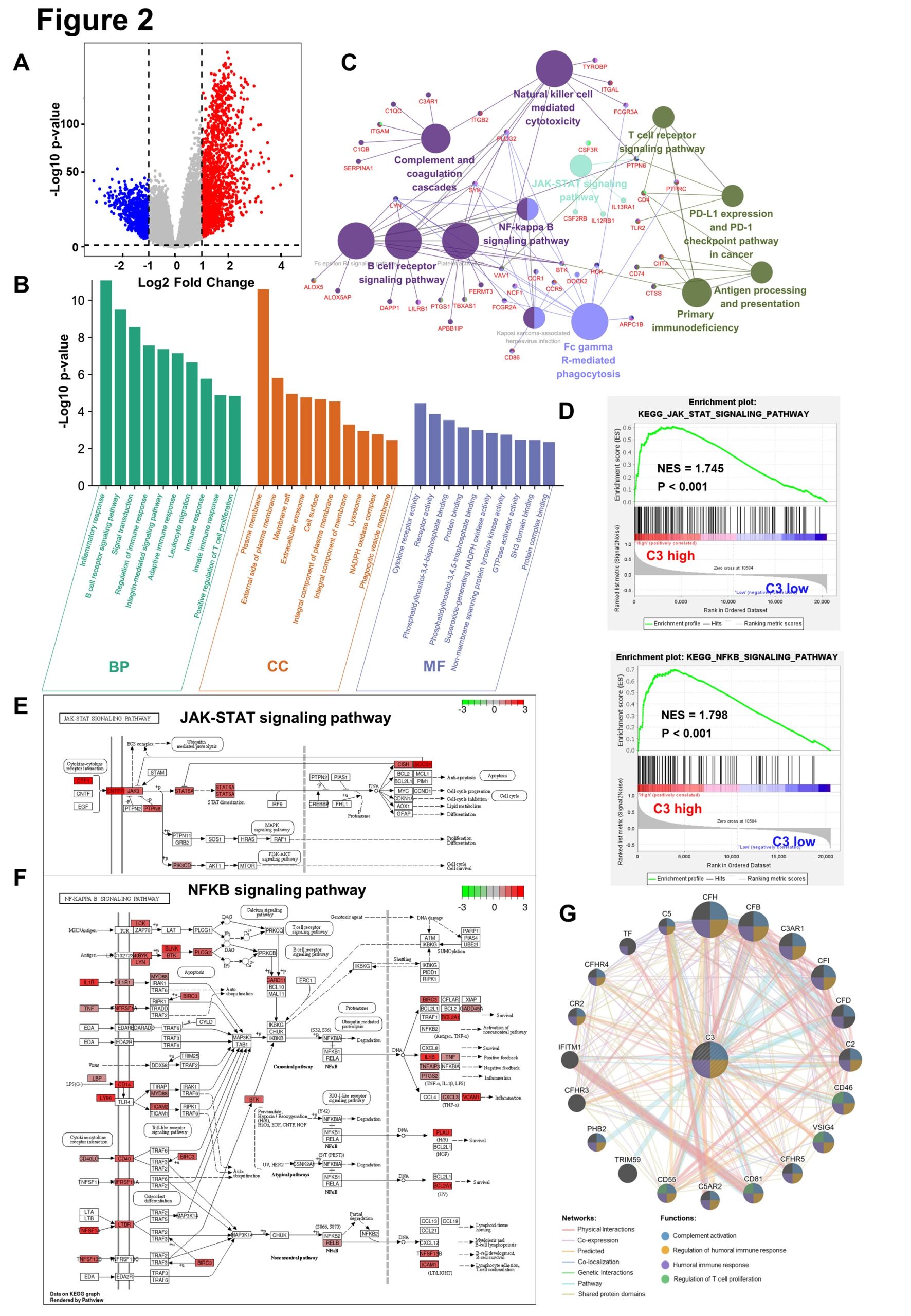
Van Herck et al. stated that 62.2% of previous studies had a positive effect on satisfaction, only 29.7% had no effect on satisfaction. Including the research of Renholm, Bryson and Browning who agree that there is an improvement in patient satisfaction. One of the potential benefits of the care pathway is to improve communication between professionals. While one study revealed that although integrated clinical pathways resulted in better health care trust, there was little evidence to suggest that interpersonal relationships and communication needed to be improved, although there was no measurable improvement. On the other hand, based on clinical results, interprofessional communication improved. Interdisciplinary teamwork can be supported by clinical pathways in other fields (Figure 2).
Figure 2: Research Model Results.
Conclusion
In this study, three important things can be found, first, the clinical quality which consists of a) patients running away, b) forced discharge, and c) readmission is highly dependent on the implementation of clinical pathways, secondly, the implementation of clinical pathways has no connection at all with costs. drug rehabilitation treatment, and thirdly the application of clinical pathways makes an important contribution to the satisfaction of patients being treated for drug rehabilitation. This means that the satisfaction factor makes an important contribution to drug rehabilitation services at the Atma Husada Mahakam Hospital.
This means that the service outcomes provided by the Atma Husada Mahakam Hospital are generally good. This can be shown by the number of high satisfaction responses from respondents to each research variable. Similarly, the service quality variable from the five dimensions has a positive and significant influence on customer satisfaction. This reinforces the previous theory that the provision of quality services can certainly create satisfaction for everyone, including the treatment of drug rehabilitation patients.
More information regarding this Article visit: OAJBGSR