Hospital Clinical Del Centro’s Patterns of Bacterial Resistance in Urine Cultures by Daniel Medina García in Open Access Journal of Biogeneric Science and Research
Abstract
Introduction: Urinary tract infection is one of the most prevalent diseases in clinical practice. They represent the third cause of morbidity in Mexico. It is advisable to carry out epidemiological studies in each hospital, at least once a year, in order to identify the current pattern of bacterial resistance and establish clinical practice guidelines for the empirical treatment of urinary infections. This study seeks to establish the pattern of antimicrobial resistance of urine cultures performed in patients with urinary tract infection to determine the most common uropathogens to guide the appropriate use of empirical antibiotic therapy. Methods: A descriptive, cross-sectional, retrospective study was carried out on the main etiological agents, the profile of sensitivity and resistance to antibiotics from urine cultures performed from urine samples of patients from the clinical hospital of the center in the city of Chihuahua, Mexico. from 2017 to 2019. Results: 214 urine cultures were analyzed, finding the most frequently isolated microorganisms were Gram-negative bacteria in 85% and Gram-positive bacteria in 15%, of which, firstly E. coli, followed by Staphylococci spp, Klebsiella spp and Pseudomonas . A general resistance greater than 75% was found for cephalothin and ampicillin; for quinolones greater than 50%, the cephalosporins: ceftriaxone (53%), cefuroxime (46.6%), cefotaxime (40.78%), cefepime (37.43%) and ceftazidime (37.43%); trimethoprim associated with sulfamethoxazole (51.8%), amoxicillin with clavulanic acid (42.11%), nitrofurantoin (28.99%) and carbapenems together with amikacin were the only antibiotics with a general resistance lower than 30%. Conclusion: The importance of the urine culture registry is extended not only in patients with recurrent urinary infections, complicated or with treatment failures, but also to maintain a local registry of the most frequent uropathogens and the antimicrobial resistance patterns of the population attended.
Keywords
Urinary infection, bacterial resistance, uropathogens, urine culture, Escherichia coli, antibiotics, cephalosporins, quinolones, general urinary examination.
Introduction
Urinary tract infection (UTI) is one of the most prevalent diseases in clinical practice, being found in both hospitalized and outpatient patients around the world [1-3] They represent the third cause of morbidity in Mexico, with respiratory and gastrointestinal infections occupying the first and second place respectively [4]. In 2017, 4,474,599 new cases of urinary tract infections were diagnosed in our country [5,6]. Except for some microorganisms that can be found in the anterior urethra, the urinary tract is free of microorganisms, therefore their presence in the urine is likely to be indicative of infection [7].
Invasion of the healthy urinary system is restricted to a very select group of microorganisms, called "uropathogens", which are capable, through the expression of virulence factors, of bypassing or minimizing the defense mechanisms of the host [8]. In general, women are more affected by UTIs than men. It is estimated that, by the age of 24 years, 33% of women will require antimicrobial treatment for at least one episode of UTI and more than 50% will experience at least one UTI during their lifetime, in fact, 75.6% of the cases of urinary tract infections reported in 2008 in Mexico were diagnosed in female patients.6 Women with a diagnosis of urinary tract infection have a 44% risk of becoming infected the following year [9-13].
The reason why the infection is more frequent in women is due to the proximity of the urethra; Furthermore, the distance between the urethra and the bladder is shorter in women and facilitates colonization of the bladder [3,14]. In women there are two stages in which the frequency of urinary infections increases: in sexually active women, since the colonization of the urinary tract is favored, and during pregnancy, since progesterone conditions the decrease in bladder emptying, due to its inhibitory effect on smooth muscle contraction, and there is compression of the ureteral system, with increased urinary stasis [15]. In men, it is more frequent in those over 50 years of age, secondary to obstruction by prostate growth. In the hospital environment, urinary tract infections are among the first three causes of nosocomial infections and are usually associated with the presence of urinary catheters [14].
Urinary tract infections are one of the most frequent abnormalities and cause of increased morbidity both in the hospital and in the community, so knowing the main isolated germs, as well as the resistance patterns, allows determining the variation that exists between the different bacterial species and guide the empirical initiation of antibiotics with greater elements of success [15].
In recent years, the number of bacteria that are resistant to first-line antibiotics has increased dramatically. It is defined as multi-resistant bacteria when there is bacterial resistance to 3 or more groups of antibiotics and pan-resistance when there is resistance to all the antibiotics of the ordinary antibiogram. Since the 1990s, Gram negative bacteria capable of producing enzymes that hydrolyze the beta-lactam ring of antibiotics began to emerge. These bacteria are called ESBL (Extended Spectrum Betalactamases) [16], These bacteria can be the cause of the infection acquired in the community in 14-31% [17,18] This has been associated in patients with a history of previous administration of antibiotics [19,20].
The frequency of pathogen isolation and bacterial resistance vary widely depending on the different geographic regions, even between hospitals in the same country and city [21]. The World Health Organization has considered the emergence and spread of antimicrobial resistance as a priority problem and therefore since September 2001 a global measure for the containment of antimicrobial resistance (Global Strategy for Containment of Antimicrobial Resistance) was instituted, which includes as a fundamental measure the surveillance of antimicrobial susceptibility [22]. That is why it is important to publish and make known the patterns and trends of sensitivity in the different hospitals of the country and the world in order to apply or intensify strict measures of surveillance and control of the use of antibiotics [15, 23,24].
In Mexico, an incidence of multidrug resistance in urine cultures of up to 22% and pan-resistance of 0.5% has been reported. In response to the appearance of these resistant microorganisms, new drugs have been developed that are resistant to the defense mechanisms of bacteria, there are also "old" drugs that continue to be effective against bacteria, such as aminoglycosides and nitrofurantoin. It is advisable to carry out epidemiological studies in each hospital, at least once a year, in order to identify the current pattern of bacterial resistance and establish clinical practice guidelines for the empirical treatment of urinary infections [20].
Knowing the main microorganisms involved, as well as the susceptibility patterns in hospital centers, allows initiating an empirical directed antimicrobial treatment, which is very useful especially for immunosuppressed patients or with data of severe sepsis [25].
There are multiple forms of presentation, from asymptomatic bacteriuria to pyelonephritis with all the signs and symptoms that can occur in different types of patients, say pediatric, elderly, pregnant, cancer patients, etc. The mechanisms by which urinary infection occurs are varied and complex and not only depend on host factors but also on the pathogenicity mechanisms that bacteria have [26]. Uncomplicated urinary infection is one that affects subjects with a structurally normal urinary tract and whose defense mechanisms are intact [8]. UTIs can be complicated by bacteremia and sepsis, which increases morbidity and mortality, length of hospital stay, and related costs. In the last decade, an increase in resistant bacterial strains in urine was identified, both from community patients and hospitalized patients [25].
The financial burden is notable, especially in Latin American countries, where the prescription of antimicrobials is less strictly controlled. A cross-sectional study conducted in a pediatric hospital in the state of Sonora, found that the average cost of medical care per episode of nosocomial urinary infection was $ 2,062.00 USD.6.
Resistance to antibiotics and appeared with the introduction of these drugs in medical institutions, and increased as it was widespread clinical use and other areas of human endeavor (livestock, aquaculture, forestry, etc.) is therefore from The emergence of antimicrobials raised concerns about the emergence of bacterial resistance to antibiotics, as was pointed out early by Fleming and Waksman (both Nobel Prize winners for discovering penicillin and streptomycin, respectively) who pointed out that their inappropriate use could generate resistance. bacterial infection in microorganisms with greater significance in the clinic and in public health, with a high risk of treatment failure [14]. The empirical use of antibiotics improperly in the treatment of UTIs can facilitate the development of resistanc to antimicrobial agents, which poses a great challenge for clinicians and researchers, since data on the prevalence of Uropathogens and antimicrobial susceptibility vary between care centers and cities and must be identified for each hospital [3, 27-29].
Due to their characteristics and virulence, uropathogens have for many years been subjected to the action of multiple antimicrobials: beta-lactams (with or without inhibitors), fluoroquinolones, aminoglycosides, furans, among others, all of them have been present at some point in the therapeutic schemes of UTIs, [20] which is why these bacteria have evolved resistance mechanisms that make them currently included within the group called ESCAPE together with such invasive microorganisms as Escherichia coli, Staphylococcus aureus methicillin resistant, Clostridium difficcile, Acinetobacter baumannii, Pseudomona aeruginosa and Vancomycin resistant Enterococcus [26].
The increase in antimicrobial resistance may be due, in small part, to the recommendation to initiate treatment empirically without the need for microbiological documentation in the face of predictive symptoms of low uncomplicated urinary tract infection [27,30,31]. On the other hand, resistance records obtained from urine culture laboratory reports tend to overestimate the true prevalence of resistance due to the selection bias inherent in the indication of these studies (patients who failed initial treatments, complicated urinary tract infections or associated resistance factors) [8,32-35] Resistance mechanisms have been thoroughly studied in E. coli and it is suspected that these are shared by the rest of the uropathogens.
Some of the mechanisms described are:
- Alterations in permeability: low level of resistance, nonspecific, although it is generally accompanied by another mechanism.
- Extended spectrum β-lactamase (ESBL): Class A (Ambler) Group 2b KB: TEM-1, TEM-2 and SHV-1 show resistance to ampicillin and ticarcillin. Inhibitable by sulbactam, clavulanic and tazobactam. Overproduction of TEM-1 or SHV-1 generates resistance to ampicillin, ticarcillin, amoxicillin / clavulanate, ampicillin / sulbactam, and cephalothin.
- Extended spectrum β-lactamase (ESBL): Group 2be KB: TEM, SHV, CTX-M, PER, VEB, GES, OXAs. They are resistant to ampicillin, ticarcillin, piperacillin, 1st, 2nd, 3rd cephalosporins (cefotaxime, ceftriaxone, ceftazidime) and 4th generation (cefepime) and monobactams. They generally have accompanying resistance to quinolones and aminoglycosides.
- Plasmid AmpC-type β Lactamase: Class C (Ambler) - Group 1 (KB). They have the characteristic of giving resistant cefoxitin, although there are exceptions. They are inhibible by oxa / cloxa and boronic acid. They generate resistance to 3rd generation cephalosporins and decrease in the sensitivity of 4th generation. In the case of uncomplicated urinary tract infection, the use of sensitive 3rd generation cephalosporins in the antibiogram can be successful in treatment [36].
- Quinolone resistance: Chromosomal mutations (non-transferable): Target site alterations (QRDR mutations of gyrA, gyrB, parC, parE genes). The main resistance mechanism in quinolones. Decrease in the cytoplasmic concentration of the drug (reduced permeability, E-flux)
Plasmid mechanisms (transferable):Protection of the target site (Qnr protein protects DNA gyrase and Topo IV) ,Enzymatic modification of ATB (enzyme AAC (6`) -1b acetylates the NH2), E-flux group specific for fluoroquinolones.
- Carbapenemases: they are classified into serine carbapenemases, metallo β-lactamase (MBL). They are enzymes that inactivate all beta-lactam antibiotics (penicillins, cephalosporins, and carbapenems). Cut-off points to suspect the presence of carbapenemase: CAZ≤22 and MER≤23 [37].
In recent years, the presence of KPC has been reported in Enterobacteria, with Klebsiella pneumoniae being the main pathogen that carries this resistance, but cases have already been detected in E. coli, C. freundii, Serratia marcescens and Enterobacter cloacae [13].
Methods
Methodological Design
Descriptive, cross-sectional, retrospective study on the main etiological agents, the profile of sensitivity and resistance to antibiotics from urine cultures performed from urine samples of patients treated in the emergency department and internal medicine of the clinical hospital of the center in the city of Chihuahua, Chihuahua, Mexico from January 8, 2017 to August 23, 2019.
Data Analysis
The following type of analysis was performed: identification of urine cultures, of drugs evaluated for sensitivity and resistance in the antibiogram , the bacteria isolated in all the processed urine cultures and the results of the antibiograms in the clinical and microbiological laboratory of the hospital were identified throughout the study period, these urine cultures were processed using the manual Chromagar technique of the supplier Beckton Dickinson Diagnostics ( BD) with calibrated loop, incubation at 37ºC for 24 hours, including those with more than 100,000 Colony Forming Units per milliliter (CFU) in the analysis.
In addition, all cultures that had their corresponding antibiogram based on the semi-automatic MicroScan autoSCAN-4 system were evaluated. Antibiotics used for the management of UTI and Gram-positive bacterial infections were included. For data analysis, the statistical package SPSS Statistics, version 22.0 (IBM, USA) for Windows was used, descriptive statistics were used as mean, standard deviation for continuous variables and percentages for categorical variables, the test was performed of Pearson's Chi-square for the categorical ones, was determined a p <0.05as a level of statistical significance, comparing the resistance and sensitivity for each antibiotic with the previous years. The protocol was submitted for approval and authorization by the president of the teaching and research committee of the Hospital Clínica del Centro in the category of research without risk, Dr. Belinda Sofía Gómez Quintana.
Table 1: Most frequently found pathogens in 329 urine cultures from patients with UTI.


Figure 1: Most frequent pathogens in the 329 urine cultures of patients with UTI.

Figure 2: General antibiotic resistance in E. coli obtained from urine cultures.

Figure 3: General antibiotic resistance in staphylococci obtained from urine cultures.
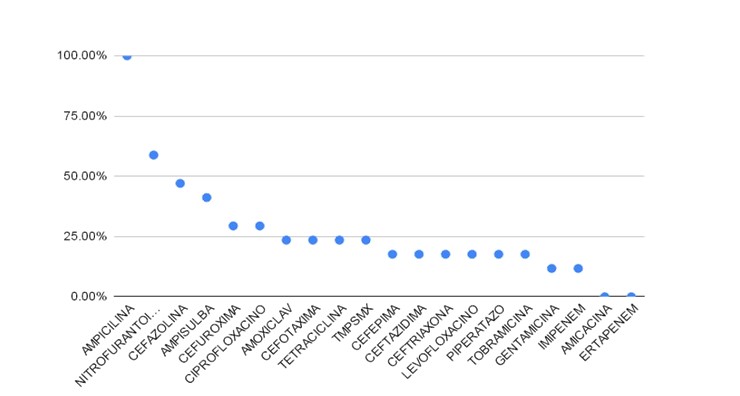
Figure 4: General antibiotic resistance in klebsiella spp obtained from urine cultures.
Results
Statistical Analysis
214 positive urine cultures were analyzed for bacterial growth, finding that the most frequently isolated microorganisms were Gram-negative bacteria in 85% and Gram-positive bacteria in 15%, of which, in the first place, Escherichia coli, followed by Staphylococci sp, Klebsiella sp and Pseudomonas As can be seenin (Table 1) and (Figure 1).
The general resistance of the analyzed cultures that were positive for E. coli, as we can analyze in (Figure 2), showed a high percentage of cephalothin (94.74%) and ampicillin (73.98 %); Antibiotics such as norfloxacin, ampicillin associated with sulbactam, levofloxacin, ciprofloxacin, cefazolin, and trimethropin associated with sulfamethoxazole, in order from highest to lowest resistance, remain between (68% and 55%). Between 50% and 40% are the second, third and fourth generation cephalosporins: cefuroxime, cefepime, cefotaxime, ceftazidime and ceftriaxone. Antibiotics such as amoxicillin associated with clavulanic acid, aminoglycosides (amikacin and gentamicin) and nitrofurantoin maintain low resistance (less than 30%). carbapenemic antibiotics (ertapenem and imipenem) show zero resistance (less than 5%).
The general resistance pattern in the cultures that were analyzed and that were positive for the staphylococcal strains, as shown in (Figure 3), we found absolute resistance to ampicillin, the antibiotics amoxicillin with clavulanic acid, ampicillin associated with sulbactam, ceftriaxone, and the quinolones ciprofloxacin and levofloxacin showed resistance between 80 and 60%. With an intermediate resistance between 55 and 30% are the antibiotics gentamicin, tetracycline, vancomycin and trimethoprim associated with sulfamethoxazole, it should be noted that nitrofurantoin shows a general resistance of only 30%, being the most sensitive for the treatment of infections urinary tract by staphylococci.
The general resistance of the analyzed cultures that were positive for the Klebsiella strains, as we can analyze in (Figure 4), showed absolute resistance to ampicillin; antibiotics such as nitrofurantoin, cefazolin and ampicillin associated with sulbactam maintain resistance between 60% and 40%. The cephalosporins cefuroxime and cefotaxime, together with amoxicillin associated with clavulanic acid, trimethoprim with sulfamethoxazole and ciprofloxacin maintain low resistances between 30% and 20%. The third and fourth generation cephalosporins: cefepime, ceftazidime and ceftriaxone, together with levofloxacin maintain resistance rates of less than 20%. Carbapenemic antibiotics (ertapenem and imipenem) and aminoglycosides (gentamicin and amikacin show very low resistance (less than 15%).
Pearson's Chi-square statistical test was performed, relating the annual resistance of antibiotics compared to each year (2017, 2018 and 2019) yielded, for the following antibioticsvalues p less than 0.05, amoxicillin with acid clavulanic(p = 0.014), cefazolin (p = 0.027), trimethoprim associated with sulfamethoxazole (p = 0.037), nitrofurantoin (p = 0.005) and piperacillin with tazobactam (p = 0.009); therefore we can reject the null hypothesis and it is established that there have been no changes in the resistance patterns during the years 2017 to 2019. The data obtained for the antibiotics amikacin (p = 0.061), tetracycline (p = 0.070), cefepime (p = 0.522), cefotaxime (p = 0.131), ceftazidime (p = 0.469), ceftriaxone (p = 0.214), cefuroxime (p = 0.225), ertapenem (p = 0.572), gentamicin (p = 0.775), imipenem (p = 0.77 5), yieldedvalues p greater than 0.05, which accepts the null hypothesis, indicating statistically significant changes in resistance patterns; however, these changes are evidently due to an increase in the antimicrobial sensitivity of uropathogens. Lastly, the antibiotics tobramycin (p = 0.427), ciprofloxacin (p = 0.469), levofloxacin (p = 0.375), vancomycin (p = 0.447), norfloxacin (p= 0.178), ampicillin with sulbactam (p= 0.347), ampicillin (p = 0.173), cephalothin (p = 0.943), showedvalues p higher than 0.05, which accepts the null hypothesis, indicating statistically significant changes, but they are demonstrated in a statistically significant increase in the resistance of uropathogens to said antibiotics through time studied.
Discussion
The results obtained highlight the fact that, as reported by surveillance studies of urinary infections from other regions of the world, gram-negative bacteria are the most commonly isolated pathogens, of which Enterobacteriaceae are the most often isolated pathogens. E. coli ranked first in isolates, albeit in a lower percentage (57.9%) compared to literature reports (~ 70%), followed by Staphylococci (10.7%) and Klebsiella third (7.9%).
A general resistance greater than 75% was found for cephalothin and ampicillin (82.35% and 78.2%, respectively) for which it is recommended not to be used as therapy for urinary tract infection. In general, quinolones (levofloxacin, ciprofloxacin and norfloxacin) presented a resistance greater than 50%, so it is advisable not to be used as first-line antibiotics in the treatment of uncomplicated urinary tract infections and that their use is restricted to administration intrahospital or under documentation of urine culture with sensitivity to these quinolones. Carbapenems (imipenem and ertapenem) together with amikacin were the only antibiotics with a general resistance lower than 25%, for which their use is recommended in patients with urosepsis. The first generation cephalosporins cephalothin (82.35%) and cefazolin (56.74%) show resistance greater than 50% and are not recommended as outpatient therapy, in addition to not having oral presentations. second, third and fourth generation cephalosporins, with the exception of ceftriaxone (53%), maintain resistances lower than 50%, of which only cefuroxime (46.6%) is found in the oral route, the rest: cefotaxime (40.78% ), cefepime (37.43%) and ceftazidime (37.43%) are only found in the parenteral route, so they should be used only in the hospital and not as outpatient treatment.
Trimethoprim associated with sulfamethoxazole (51.8%) maintains relatively high general resistance, however the resistance for E coli increases to 55.75%, compared to the resistance, less than 50%, that it presents for Klebsiella and staphylococci (23.53% and 36.36%, respectively). Amoxicillin with clavulanic acid (42.11%) maintains a resistance lower than 50%, it is in oral presentation and maintains low resistance for bacteria such as E. coli (30.89%) and Klebsiella spp (23.53%), however it maintains a resistance high for Gram-positive bacteria, such as streptococci (78.26%) and enterococci; Therefore, its use is suggested empirically for urinary tract infections when it is suspected that the uropathogen belongs to the Gram-negative group. Nitrofurantoin (28.99%) maintains a low resistance rate in general, is found in oral therapy and should be used in urinary tract infections with failure prior to treatment, with or without urine culture that confirms the sensitivity of the uropathogen, or in patients with recurrent urinary infections.
Resistance of E. coli to drugs frequently used in outpatients with urinary tract infections, such as ciprofloxacin and levofloxacin, was recognized as alarmingly high (60.98% and 61.48%, respectively); Consequently, it is possible to conclude that due to this high rate of resistance, these drugs should be left out of the arsenal of empirical therapy for urinary tract infections in the community and only be used for complicated or intrahospital urinary tract infections. Nitrofurantoin (11.76%) remains with a low resistance, which is why it should be the initial therapy in patients with recurrent symptoms, with or without urine culture that confirms the sensitivity of the uropathogen.
More information regarding this Article visit: OAJBGSR

No comments:
Post a Comment