Feasibility Review of Wearable Kinematic Sensors in Post Knee Arthroplasty Patients by Allan Le* in Open Access Journal of Biogeneric Science and Research
Abstract
Introduction: Post-operative surveillance of joint range of motion after knee arthroplasty is a necessity. However, as the number of these surgeries increase, there has been a significantly increased burden to have sufficient follow up. In this light, the primary purpose of this study was to assess feasibility of novel wearable kinematic sensors in detecting patient mobility limitation compared to clinical and goniometer measurements in post knee arthroplasty patients. A secondary objective of the study was to identify gaps in goniometry used in typical current follow up protocol for this population.
Methods: Two separate searches were conducted to fulfill the two objectives of this study. The databases of Medline, PubMed and Cochrane library were searched using medical subject headings and keywords during August 2020. Titles and abstracts were screened based on specified inclusion criteria and then full text reviewed.
Results: The search for the feasibility of wearable kinematic sensors yielded seven studies after screening. The search for gaps in goniometry yielded five studies after screening and full text review.
Discussions: It was found that limitations with traditional goniometry involves user experience dependence, end digit preference and poor inter-rater reliability. Wearable sensors have the advantage over goniometry in the areas of objectivity, continuity, better supervised recovery and the measurement of multiple parameters in parallel. Current limitations with these sensors are the concerns with privacy regarding GPS data and loss of data. Furthermore, the requirement of recalibration and relative sensor drift are a significant issue. Measurement of the operated leg does not give a holistic picture of gait and sensors only on the forearm can only be used to measure daily activity. Future avenues with this technology include adjunct telerehabilitation, recording subjective in parallel to objective data and using multiple sensors on both lower limbs.
Conclusion: The study demonstrated that it is feasible and advantageous to utilize wearable kinematic sensors to monitor the post-operative period of knee arthroplasty patients.
Keywords: Wearable electronic devices; knee arthroplasty; mobility limitation, goniometer
Introduction
Knee arthroplasty is one of the most common orthopedic procedures due to the high prevalence of knee cartilage pathologies such as osteoarthritis, rheumatoid arthritis and post-traumatic degenerative joint disease. In the year between 2017 and 2018, there were 54102 knee arthroplasties performed on patients who had a principal diagnosis of osteoarthritis and the incidence is steadily increasing [1]. Joint replacement remains as one of the most clinically successful and cost-effective treatments for severe osteoarthritis of the knee [2]. However, flexion contractures are a common deformity for these patients [3]. Limitations in post-operative joint mobility is established as a successful surrogate metric to predict the formation of flexion contractures. However, there remains a lack of tools to objectively measure activity and kinematic data to monitor patients in the post-operative period.
The current follow-up schedule is variable, but the typical protocol of post knee arthroplasty involves clinical measures of mobility and range of movement (ROM) measurements. These are performed by a physiotherapist who uses tests such as the timed up-and-go (TUG) and a goniometer to measure ROM. Nevertheless, a significant number of patients prefer not to come into clinics if asymptomatic [4]. Over the last few years there have been innovations in novel wearable kinematic sensors. These devices can provide objective knee kinematic data such as activity level and ROM which can potentially bridge the gap in patient monitoring in asymptomatic patients. However, there has been a paucity of evidence on the feasibility of this technology.
The lack of uptake of wearable kinematic sensors is due to a few reasons. Given the novelty of this technology, there is a dearth of research in the area. There are many different sensor types available that measure different data. This technology typically consists of one or two sensors such as: accelerometer, gyroscope, barometer, magnetometer, thermometer or pedometer. Therefore, given the breadth of sensors available and the limited research on their feasibility in the post-operative period, the aim of this review is to help facilitate their use in clinical practice.
The primary objective for this review was to investigate the feasibility of wearable kinematic sensors in detecting patient mobility limitation compared to clinical and goniometer measurements in post knee arthroplasty patients. A secondary objective was to identify gaps with goniometry performed in the post-operative follow up period.
Methods
The online databases of Medline (Ovid), PubMed and Cochrane library were searched during August 2020 using Medical Subject Headings (MeSH) and keywords. Searches were limited to systematic reviews, meta-analyses, randomised control trials, clinical trials and cohort studies. No time limit was assigned given the limited literature in the area.
Two separate searches were conducted to fulfill the two different objectives of this review. The inclusion criteria for the first search involving the feasibility of wearable kinematic sensors in detecting patient mobility limitation were: must include wearable device, must include post-operative participants, assessing patient mobility and written in English. The inbuilt sensors in mobile phones were also considered a wearable device if they were kept on the participants person and physical activity was accepted as a measure of participant mobility. The inclusion criteria for the second search involving gaps with goniometry were: must have used a goniometer to measure ROM, must include post-operative participants and written in English.
Further, hand searching was conducted in the reference lists of manuscripts for additional studies. The full search history for the primary and secondary objectives are presented in (Tables 1 & 2) of the appendix. Studies were first screened on basis of title and abstract for inclusion criteria and the remaining studies were full text reviewed.
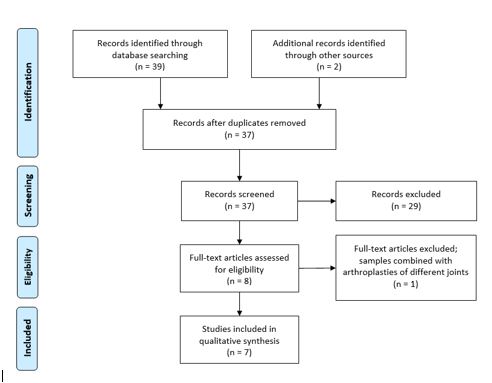
Figure 1: PRISMA flow diagram search for the feasibility of wearable sensors.

Figure 2: PRISMA flow diagram search for gaps with goniometry.
Table 1: Medline search history.
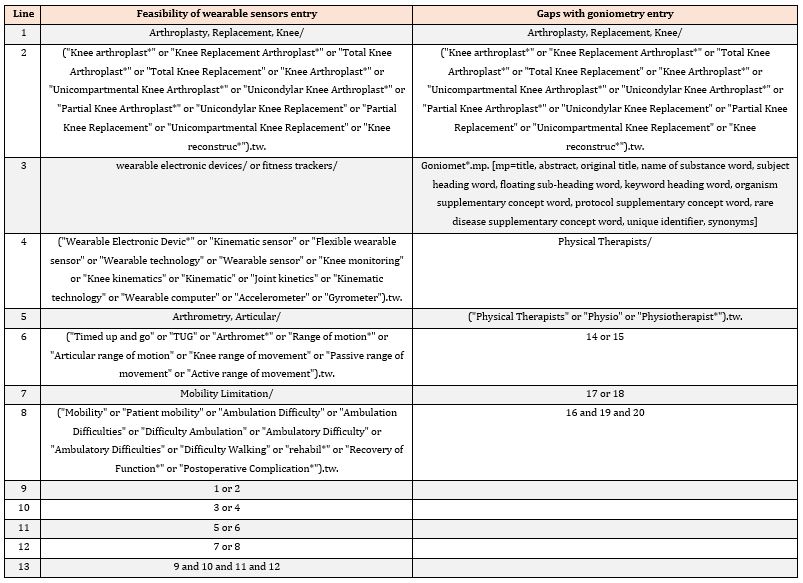
Table 2: PubMed and Cochrane library search history.

Table 3: summary of findings of studies involving wearable kinematic sensors in post knee arthroplasty patients.

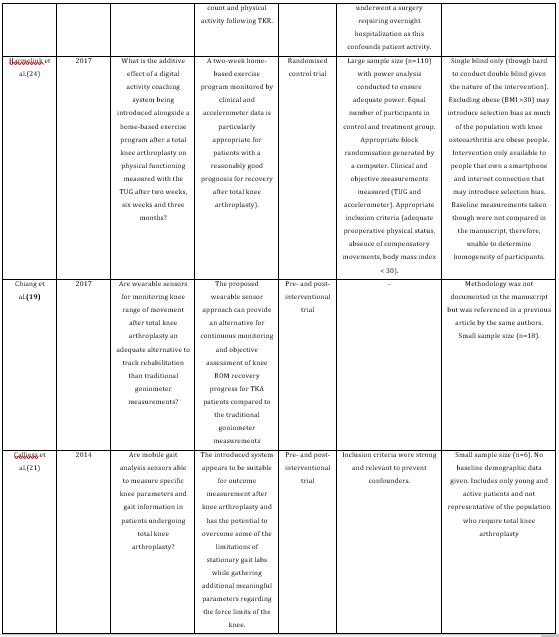
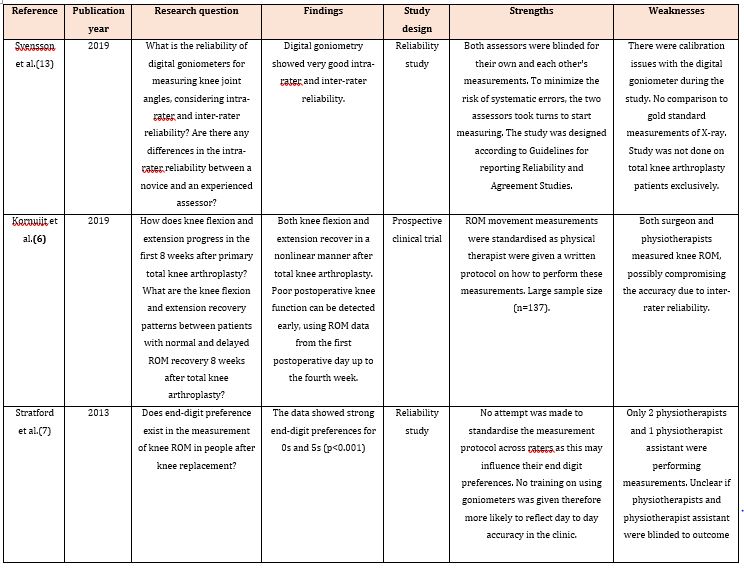
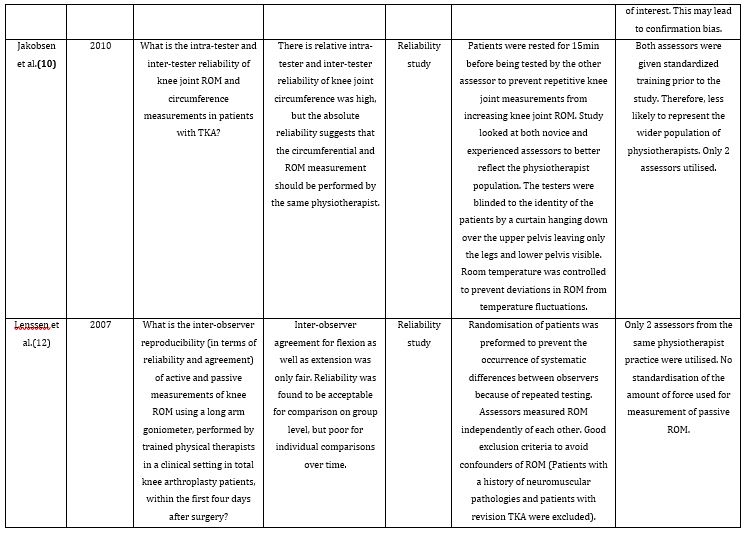
Table 4: Summary of studies involving goniometry in post-arthroplasty patients.
Results: (Figures 1 & 2)
A summary of the identified study’s findings can be found in (Tables 3 & 4) of the appendix.
Discussion
Current follow up and monitoring of rehabilitation protocol
In the post-operative period after discharge from hospital, there is high variability on the follow-up and rehabilitation protocol. There is no apparent consensus on the ideal frequency, duration or intensity of the rehabilitation protocols which are hospital and surgeon specific [5]. The typical follow-up period involves a wound review by a nurse, physiotherapist or surgeon within two weeks following the surgery. The next time the patient will see the surgeon is at six to eight weeks after the surgery with or without weight bearing radiographs of the knee. During these sessions it is likely the physiotherapist will perform ROM measurements of both knees using a goniometer and some conduct clinical measures of mobility such as the TUG.
This typical follow-up protocol only allows two points in time where the patient can interact with medical staff over a 6–8-week period. Following this point in time, follow-up is highly variable. With many of the possible post-operative complications arising in this period, there is a necessity to be able to continuously monitor patients to avoid preventable complications.
Goniometry
Goniometric measurements are one of the kinetic metrics used to monitor rehabilitation in knee arthroplasty patients. It uses a goniometer to measure ROM at the fulcrum of a particular joint. ROM of a joint is an important proxy for overall joint function. The study by Kornuijt et al [6] found that low ROM measurements taken from the first operative day up to the fourth week can predict poor knee function. Though, goniometry requires an experienced user and the patient to attend the practice for measurements to be taken.
Access to services related to rehabilitation can be a problem to those who live outside metropolitan areas. Furthermore, travel times to practices may also inhibit patients from attending their specified outpatient appointments. This is especially the case when patients rather not attend their designated appointments when asymptomatic [4]. Though, it brings into question the reliability of a patient to assess their own mobility after surgery. Patients are not trained to look for possible complications in the rehabilitation period. Therefore, it is important that kinematic data can be obtained without the requirement of the patient attending outpatient appointments. This represents a weakness with the current follow-up protocol.
Limitations in the post-operative period involves ROM measurements that are prone to biases. Subjectivity in relation to goniometry involves the preference for specific end-digits. The study by Stratford et al [7] demonstrated that the physiotherapists of varying experience had a strong end-digit preference of 0 and 5. This notion has the capacity to compromise the validity of clinical decisions; for example, if a patient has improved ROM from their last visit. There have been many studies looking at goniometer reliability which have found that inter-rater reliability is generally worse than intra-rater reliability [8-12]. Though there have been improvements in reliability with the introduction of digital goniometers [13]. they still depend on an experienced user to take the measurements.
With the limited outpatient appointments these patients receive, it is more difficult to see trends of decline or improvement. With the existing follow-up protocol, the patient will get two instantaneous measurements over a 6–8-week period. With only two points for reference, the latest measurement can only be compared to one other point 4-6 weeks earlier. Given the lack of ability to obtain trend data, it makes it harder to make the clinical decision if a patient’s mobility is truly improving, declining or plateauing.
To follow up post-operative patients requires experienced staff and sometimes the surgeon to perform goniometric measurements. This increases the staff burden and resources that could be used elsewhere in the patients’ rehabilitation. Long term surveillance of joint mobility after knee arthroplasty is a necessity but as the number of these surgeries steadily increase, it has also become increasingly burdensome to have adequate follow-up [14].
Wearable Kinematic Sensors
Sensors to monitor organ health that can transmit data wirelessly to a doctor or care team has already become the norm and well established in other areas of medicine. For example, real-time arrythmia detection in cardiovascular patients that can wirelessly transmit data to their cardiologist [15]. With the introduction of novel wearable sensors, with the specific purpose of monitoring kinematic data, offers the opportunity for utilisation by orthopedic surgeons or physiotherapists.
There is a large breadth of wearable sensor types that measure different kinematic parameters. On the simpler side of the spectrum, a study developed a smartphone app to monitor physical activity as a surrogate for improvements in knee function [16]. With growing public interest in fitness tracking, many commercial activity trackers have also become available. One of these commercial sensors, Fitbit (San Francisco, USA), was utilised by Losina et al [17] and Kline et al [16] to track physical activity. Duration and intensity of physical activity, tracked by steps taken, was used by these authors to substitute traditional clinical measures such as the TUG. The disadvantage of commercial sensors is that authors are not able to access algorithms used to calculate kinematic metrics. Furthermore, there have been developments in more complex wearable sensors that are attached to the lower limb. Ramkumar et al [18] investigated the use of a wearable knee sleeve. The device has the ability to continuously measure steps and ROM which requires pairing via Bluetooth to a smartphone. By contrast, alternate approaches have been taken by both Chiang et al [19] and Huang et al [20] who attached a sensor above and below the knee to obtain the angle between the fulcrum. By comparison, Calliess et al [21] utilised a sacral sensor in addition to two lower limb sensors.
Wearable sensors have multitudes of benefits over goniometric measurements in the post-operative period. The proposed sensors do not have the same subjectivity of end-digit preference and inter-rater reliability issues inherent to standard goniometry. Additionally, the information obtained from these sensors are objective kinematic data. Furthermore, it is possible that simple metrics such as step taken per day can be viewed by the patient themselves. This has the potential to motivate and engage patients to adhere to rehabilitation programs via the Hawthorne effect. This effect refers to when patients alter their behavior when they are aware, they are being observed [22] therefore, aiding in rehabilitation in the crucial eight weeks following a surgery.
The wearable sensors also offer the opportunity for surgeons and physiotherapists for a better supervised recovery of their patients. With typically only two follow-up appointments in the first eight weeks following surgery, most of the post-operative recovery occurs out of sight of the care teams [18] With the technology that enables continuous measurements of kinematic data, the supervision of recovery is no longer spatiotemporally constrained [20]. This allows trends to be observed beyond the typical two points in time that traditional goniometry offers. Furthermore, the data has the potential to monitor patient adherence and problems in their prescribed rehabilitation programs. As more instances in the patient’s recovery can be tracked, it is more likely that limitations in mobility can be detected than traditional goniometry.
Often, there can be multiple factors in the development of non-favorable post-operative complications of knee arthroplasty. Unfavorable outcomes in mobility and joint function may be related to the surgery itself or patient therapy non-adherence. The proposed technology gives surgeons and physiotherapists the ability to identify the potential causes of adverse outcomes despite a well-executed recovery plan and expectation management [18].
Wearable sensors are capable of measuring multiple parameters in parallel. This allows the surgeon to improve patient evaluation with no additional effort [18] Furthermore, the surgeon would be able to receive a variety of metrics such as joint specific ROM and physical activity for a more holistic picture of joint and mobility limitation of the patient. Since kinematic measurements can be taken continuously and in parallel, less staff need to be trained and allocated to obtaining this data in the surgeon’s clinic. This leads to saving both the patient’s and surgeon’s time by decompressing the clinic [18] In this light, the wearable technology presents the opportunity for reductions in human labor and financial savings.
While there are many benefits in using these novel wearable sensors, there are limitations and issues with the current technology. Commercial and some of the sensors mentioned in this review must communicate with a smartphone to be able to accurately calculate physical activity. As the patient’s location is tracked via GPS, there is the potential for breaches in patient privacy. Furthermore, as the data is initially stored on the patient’s smartphone, it is possible for data to be lost. There must be systems in place for frequent and reliable synchronisation to prevent data loss such as storing in the cloud. There are also concerns with data loss with the battery life of the sensors if they are unable to transfer data before losing power.
An inherent weakness for wearable sensors is the requirement for calibration of the equipment. The system used by Chiang et al [19] could be self-calibrated by the patient to confirm the accuracy of the data obtained by the sensors. Though, this method of calibration may not be ideal for all patients as some may need assistance from medical professionals. The frequency of calibration needed depends on the method the sensors are attached to the body. Sensor drift was a significant issue for Huang et al [20] and Chiang et al [19] who used Velcro and elastic belts. By contrast, Callies et al [21] utilised therapeutic tape to secure the sensors on the patient to prevent any significant relative motion between the sensors, thus, affecting data accuracy. This guarantees stable and defined sensor position. However, securing the sensors with tape means that the patient must continuously wear the sensors as taking them off would require further re-calibration. There are also issues on when to charge the devices, particularly with the commercial sensors which typically require charging every 3-4 days. It would be ideal to charge the devices at night when the patients are sleeping, although, this would require re-calibration when remounted.
All the proposed sensors in the reviewed studies utilize only one limb to gather data. The sensors are not able to differentiate between the knee that was operated on and the knee that was not. In this light, no data can be obtained and no inferences can be made about the non-operated side [21]. By contrast, in the studies that utilised the commercial sensors, the device was mounted on the patient’s forearm [16, 17]. In this approach, the forearm’s movements act as a proxy for the patient’s physical activity and overall joint function. However, it must be mounted on the user’s non-dominant hand to minimize the amount of upper-limb motion independent of the lower limbs. Even so, it is not the perfect substitute metric as movements of the upper limb differ greatly to the lower limb.
The wearable sensors wirelessly transmit the obtained data for storage. This is commonly to a smartphone device. The Mobile Consumer Survey 2019 found that 11% of Australians do not own a smartphone device [23] Given this notion, it is likely that those of lower socioeconomic status would not be able to access this platform. This is especially the case if they have travelled from rural areas to receive treatment which have limited internet access. Therefore, there is the possibility to worsen firmly established health disparities [18]
Further Research and Future Prospects
Recommendations for future avenues with this technology involves the use of continuous kinematic measurements in conjunction with telehealth rehabilitation programs. With the ability to monitor a patient’s recovery from a distance, patients now have the opportunity to participate in their rehabilitation programs from their homes. This is especially valuable when access to healthcare is limited by distance. This was the objective of Kline et al [16] who aimed to improve physical activity through adjunct telerehabilitation and address the gap in conventional rehabilitation. Furthermore, Losina et al [17] examined the feasibility of telephonic health coaching where physiotherapists have the ability to coach patients via video call. By contrast, Harmelink et al [24] investigated the additive effect of a digital activity coaching system introduced alongside a home-based exercise program to remove the requirement of intervention by medical staff in a patient led rehabilitation.
As many of these wearable sensors communicate with the patient’s smartphone, it is possible that other subjective data could be monitored in parallel with kinematic data. Through the development of smartphone applications, a patient can log subjective parameters to their surgeon or treating team such as pain related parameters. Development of such applications might also involve an inbuilt telerehabilitation function so patients can access all their needs from a single platform. Gathering a broad range of objective and subjective data can add to a more holistic and detailed understanding of the patient’s recovery.
In the field of multiple sclerosis, there has been the introduction of similar wearable technology. These inertial sensors are mounted on both lower limbs and the lower back therefore able to measure kinematic data from both legs [25] Given the increased number of sensors utilized, more parameters are able to be monitored for better gait analysis. Furthermore, these sensors are integrated into adhesive thus able to be mounted directly on the skin. This alleviates the common issue of relative sensor drift of elastic band mounted sensors used in the reviewed studies.
Conclusion
This review demonstrated that the recent development of wearable kinematic sensors is a feasible alternative to classical goniometric measurements and clinical measures of mobility obtained by physiotherapists. A review of all the latest research has yielded there are gaps with classical goniometry in the post-operative period such as end-digit preference and user experience dependency. The research suggests that the breadth of both objective and subjective parameters that can be gathered through wearable sensors eclipses the amount of data that can be obtained in the current follow up protocol. Despite this, there are significant issues with the current technology such as the need for frequent recalibration and relative sensor motion. This represents the necessity of further investigating approaches to counteract these limitations. The studies examined in this review demonstrate the large scope of novel sensors available, therefore, more research must also be conducted on individual sensors.
Conflict of Interest Statement
Each author certifies that they have no commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements, etc.) that might pose a conflict of interest in connection with the submitted article.
More information regarding this Article visit: OAJBGSR

No comments:
Post a Comment