Predicting Abnormal Medical Tests, on a Symptom-by-Symptom Basis, Using the Large Analytic Bayesian System (Labs): A Bayesian Solution Applied to Diagnostic Test Management by Nelson Hendler* in Open Access Journal of Biogeneric Science and Research
Abstract
Earlier research described the development of a Large Analytic Bayesian System (LABS) which uses Bayesian analytics to list, on a symptom-by-symptom basis, the likelihood of having abnormal medical testing from a list of possible medical tests associated with a symptom, or cluster of symptoms. LABS produces a rank ordered list of medical tests, comparing the symptom(s) with the frequency and severity of abnormal medical tests. Seventy-eight medical charts with evaluations including all pertinent medical tests, and a completed Diagnostic Paradigm with 2008 possible symptoms were reviewed. On a symptom-by-symptom basis, medical test results in the chart were compiled using the Large Analytic Bayesian System (LABS) and created a rank ordered list of abnormal medical tests from a list of possible 107 medical tests. This resulted in a 2008 by 107 matrix, which was analyzed by the use of a program called the Diagnostic Test Manager. The results clearly demonstrated that physiological testing, such as root blocks, facet blocks and provocative discograms had nearly double the frequency of abnormalities compared to anatomical tests, such as X-ray, CT scans and MRIs in the same patient. This evidence-based approach will help physicians reduce the use of unnecessary tests, improve patient care, and reduces medical costs.
Introduction
The medical literature abounds with articles which report a misdiagnosis rate ranging from 35% to 67% for a variety of disorders, including pneumonia, and heart disease, low back and neck pain, and headache (25, 4, 5, 15). Primary care physicians missed 68 out of 190 diagnoses (35%) according to a 2013 study, with pneumonia and congestive heart failure the most commonly missed (1). The two leading causes for misdiagnosis were ordering the wrong diagnostic tests (57%), and faulty history taking (56%) [1].
Diagnostic errors lead to permanent damage or death for as many as 160,000 patients each year, according to researchers at Johns Hopkins University [1]. Not only are diagnostic problems more common than other medical mistakes-and more likely to harm patients-but they're also the leading cause of malpractice claims, accounting for 35% of nearly $39 billion in payouts in the U.S. from 1986 to 2010, measured in 2011 dollars, according to Johns Hopkins [1].
Misdiagnoses of some diseases range from 71% to 97% (RSD, electrical injuries, and fibromyalgia) [2-5]. This high rate of misdiagnosis is costly to insurance companies and other payers, as well as to employers of chronic pain patients, where 13% of the workforce loose productive time, estimated to cost industry $61 billion a year [6]. Furthermore, misdiagnosis creates protracted treatment and psychological problems for the patients themselves. Of all the misdiagnosed disorders, the most prevalent problem is chronic pain, which, according to the Academy of Pain Medicine, accounts for 100,000,000 patients in the United States alone [7]. The annual cost of health care for pain ranges from $560 billion to $635 billion (in 2010 dollars) in the United States, which includes the medical costs of pain care and the economic costs, related to disability, lost wages and productivity [7].
Insurance companies and physicians could improve patient care if they had a mechanism which would address the two-leading cause of misdiagnosis: faulty history taking and ordering the wrong medical tests. [1]. Therefore, a valuable tool for any health care system would be a questionnaire which could provide accurate diagnoses, and, based on the accurate diagnoses, predict the outcome of an expensive medical laboratory tests, to allow physicians to determine, using “evidence-based medicine,” which tests would be diagnostic and which test would be of no value. This concept is best exemplified by the Ottawa Ankle Rules, and Ottawa Knee Rules, developed in Canadian emergency rooms. They developed a questionnaire, using “predictive analytic techniques,” which could predict which patient would or would not have abnormal ankle or knee X-rays. When the use of the Ottawa Ankle and Knee Rules was applied in emergency rooms, for the selection or denial of patients for ankle or knee X-rays, it decreased ankle and knee radiography up to 26 percent, with cost savings of up to $50,000,000 per year [8-11]. This significant savings was just in the city of Ottawa, and just for ankle and knee pain. If these techniques were applied to other cities and other conditions, the extrapolated savings would be billions of dollars a year.
Later research by the group from Ottawa focuses demonstrated that expert system evaluations, based on predictive analytic research, which were more accurate in predicting the results of cervical spine X-rays, and CT, than unstructured physician judgment [12-14]. These same “predictive analytic” techniques allowed physicians from Mensana Clinic and Johns Hopkins Hospital to develop a Pain Validity Test which could predict with 95% accuracy which patient would have moderate or severe abnormalities on medical testing, and predict, with 85% to 100% accuracy, who would have no abnormalities, or only mild ones [15-18].
Past research reports from Mensana Clinic indicate that 40% to 67% of chronic pain patients involved in litigation are misdiagnosed [19,20]. When evaluating complex regional pain syndrome, (CRPS), formerly called reflex sympathetic dystrophy (RSD), Hendler found that 71% of the patients, and Dellon found that 80% of the patients, who were told they had only CRPS I, actually had nerve entrapment syndromes (2,3). These errors in diagnoses are costly to the patient and the insurance industry alike, since they prolong or result in inappropriate treatment.
Most physicians use an MRI, which is test used to detect anatomical abnormalities, to determine disc damage in the spine. However, the medical literature shows that the MRI has a 28% false positive rate, and a 78% false negative rate for detecting spinal disc damage, compared to a provocative discogram. [21,22]. Therefore, the physicians from Mensana Clinic and Johns Hopkins Hospital supplemented the anatomical MRI findings with physiological testing, such as provocative discograms, facet blocks, and root blocks, which are typically not used by most physicians. Donlin Long, MD, PhD, former chairman of neurosurgery at Johns Hopkins Hospital, used these physiological tests in a group of 70 patients who previously had normal MRI, CT, and X-ray (anatomical tests), and were told by their treating doctors that nothing more could be done to help these patients. When properly diagnosed, 95% of the patients required physiological testing, and 63% required surgery [23]. Using these techniques, 93% of the patients receiving good to excellent relief after proper diagnosis and correct surgery [23]. Additionally, Johns Hopkins Hospital saved 54% a year on its workers’ compensation expenses, with the simple expedient of having all of Johns Hopkins Hospital employees injured on the job seeing only Johns Hopkins Hospital doctors [24], instead of physicians in the local community, where the misdiagnosis rate was 40-71% [2, 19,20].
The Maryland Clinical Diagnostics (MCD) Diagnostic Paradigm is a questionnaire, containing 72 multi-part questions, with 2 to 74 possible responses to a question, for a total of 2008 possible answers. These questions duplicate the questions asked during an evaluation process for a patient with chronic pain, by former faculty members from Johns Hopkins University School of Medicine. Asking these questions and recording answers to these questions can take a physician 50 to 60 minutes to complete. The test is then computer scored and interpreted. The MCD Diagnostic Paradigm questionnaire is administered over the Internet (www.MarylandClinicalDiagnostics.com).
Each answer is scored on a spread sheet. The Maryland Clinical Diagnostic Paradigm was designed to detect 60 diagnoses and 44 differential diagnoses most commonly seen after workers’ compensation and auto accident (post-traumatic) injuries. In a published research report, the MCD Diagnostic Paradigm accurately replicated the diagnoses made by staff members of Johns Hopkins Hospital staff members 96.2 % of the time [25]. The validity of this test is borne out by outcome studies which report that the diagnoses from the Diagnostic Paradigm and Treatment Algorithm can predict intra-operative findings with 100% accuracy [26].
Historically, physicians take a careful history, derive a diagnosis and differential diagnosis, and use medical testing to confirm or reject the various diagnoses. However, a shift in the medical evaluation paradigm has occurred. Physicians are now relying more on medical testing rather than a careful history. In fact, the time a physician spends with patients averaged 11 minutes, with the patient speaking for about 4 minutes of the 11 minutes [27] Therefore, this increasingly prevalent process, which we deplore, follows the format of first getting a list of the symptoms, then getting medical testing pertinent to the symptoms to establish or eliminate diagnoses, and finally reaching a diagnosis, i.e., using medical testing to make a diagnosis. Unfortunately, with an inadequate history, the chance of an erroneous diagnosis increases, leading to the selection of incorrect medical testing. The technique we describe augments the latter paradigm of truncated history taking, and provides evidence-based medicine for selecting the correct medical test, to supplement inadequate history taking.
Methods
For decades, traditional database application design approaches were attempted to classify and organize large amounts of available medical data. Our Bayesian approach offers a solution to a dilemma faced when the authors attempted to categorize and rank this statistically congruent data group of 660,000,000 data points presented for analysis. This data group is simply too large and complex for a standard database application. To manage that amount of data would require terabytes of dynamic storage, thus making a Bayesian type solution for even the largest of computing platforms impractical. A new application, titled Diagnostic Test Manager, is the result of recent developments in science and machine intelligence, which involve computer aided process optimization. This new approach allows Diagnostic Test Manager or DRM, to be hosted on a typical PC desktop computer with rapid, almost instant, response and analysis.
For this evidentiary predictive application, the authors randomly selected 78 completed Mensana Clinic medical charts as a starting point during the software application development and functional demonstration phase. The completed medical charts included a patient symptom questionnaire (Diagnostic Paradigm) with 72 questions, and a total of 2008 possible multiple-choice answers which rate the type, frequency, and location of the patient’s pain. As a result of the diagnoses reached by evaluating these symptoms, there were 107 medical tests which could be administered. The medical test results were ranked from Within Normal Limits (WNL), Mild, Moderate, or Severe/Abnormal indications. It should be noted that doubling the number of charts of the initial group, which represented 147,000,000 data points, increased the predictive accuracy of DRM by only ~2%. Mensana Clinic (which Business Week listed as one of the top 8 best pain centers in the United States, along with Mayo Clinic, Cleveland Clinic and Johns Hopkins Hospital) [28], was operated by Johns Hopkins Hospital staff members, who ordered sophisticated laboratory tests not commonly ordered by other physicians. This resulted in a collection of medical data that is not typically available at almost any other medical center or from treating physicians. It is highly unlikely that the data obtained from these charts can be duplicated. Thus, the results of the process are unique, exhaustive, and proprietary.
DRM accumulated all the answers to the Diagnostic Paradigm for all 78 patients. The range of affirmative answers was 18 to 1,237 of the 2008 possible answers, depending on the type of injury the patient sustained. If the patient only had a nerve entrapment in the wrist, the patient had very few positive answers to the questions. On the other hand, if the patient has been in a severe automobile accident and had pain in the neck, both arms, and both legs, the patient would have many more answers to the questions. DRM listed all the positive answers to the Diagnostic Paradigm which had been marked by all patients. Obviously, for the most common type of injury there would be more data points for certain answers, since there would be more patients with those symptoms.
Fifty-two of the patient charts represented patients with a complete evaluation with all recommended testing completed, while the remaining charts represented patients with at least 50%-95% of all recommended tests completed. Charts with less than 50% of the tests completed were not included in this research. Also, excluded from the research sample were patients who had only an evaluation, but no medical tests, patients who had less than 50% of the recommended testing performed, patients who had a chronic pain problem which was not covered by the diagnostic assessment of the Diagnostic Paradigm, such as genital pain, facial pain after a face lift, rectal pain, or nipple pain after breast augmentation.
The DRM showed the specific medical test results, of the 107 possible medical tests, which were administered to each patient. DRM associated these medical test results to the answers for each of the patients. The basic logic is that patients who responded to symptom questions are going to have a similar spectrum of test responses. This forms evidence-based data for optimal test performance decisions. These data can be displayed using histograms, for visual recognition, and a simple Excel spread sheet, for a numerical representation. DRM automates the assessment of a benchmark instrument which compiles a matrix comparing the answers on the MCD Diagnostic Paradigm to the results of the medical testing, in much the same manner the Ottawa Ankle and Knee rules did for ankle and knee X-rays, and the Pain Validity Test did for objective medical testing in chronic pain patients. However, DRM provides a broadly expanded clinical set of data.
Based on this analysis, a data base is created which rank orders the likelihood of a test being positive for a given set of symptoms. The data organization for this reporting process is straight forward and simply the recordation of a specific question’s choice. The data storage action accumulates all of the patients’ medical test results for each of the specific answers. This resulting evaluation is a numerical count of the medical test abnormalities found for each answer. The number of abnormal medical tests associated with each of the possible answers can be displayed as a graph or refined into a MS Word/Excel compatible report.
Results
The DRM results revealed the rank ordered tests, from most frequently abnormal, to least frequently abnormal for each symptom a patient had for all 75 patients. Clusters of symptoms typically seen for the most common diagnoses also were evaluated. Some of the most common diagnoses symptoms and the abnormal medical test rank order are shown below in (Table 1). The percentage represents the number of abnormal tests obtained for a patient with a specific symptom as a percentage of all tests of that type performed on a patient with that symptom. There are various reasons that not all of the patients with certain symptoms received all of the appropriate testing:
- Insurance would not pay for the procedure,
- The patient was afraid of the interventional testing,
- The test could not be scheduled before the patient departed,
- There were anatomical abnormalities which prevented the insertion of a needle into a disc space,
- There was no clinical indication to order a provocative discogram, for example because just neck pain is not associated with discogenic neck pathology . Therefore, only the actual number of patients receiving the test is recorded and is represented by the N which follows the type of test.
There are two ways to represent the results of this comparison. The first is a frequency histogram, and the second is an Excel spread sheet. (Figure 1) below represents the frequency histogram for all medical test results for the single symptom, “My neck pain is constant.” There are many etiologies to this single symptom, such as a herniated disc, thoracic outlet syndrome, radial nerve entrapment, cervical radiculopathy, and cervical facet syndrome, to name a few. This accounts for the variety of abnormal medical tests for just a single symptom. Additionally, a patient may have more than one symptom, and symptoms related to other areas of the body. A patient injured in an auto accident may have neck and back pain but the frequency histogram reports all abnormal test a patient has, even though just one symptom is being examined.

Figure 1: Frequency histogram of all abnormal medical tests associated with a single symptom.
Table 1: For Symptom: My Neck Pain is Constant.

(Table 1) below shows these data in an Excel format of abnormal tests for a single symptom, eliminating abnormal tests for the lower body, for the sake of clarity. Auto accident cases frequently have hyperextension injuries, which produce thoracic outlet syndrome, and accounts for the high level of abnormal vascular flow studies in the arms, when in Roos position. This position detects post-traumatic vascular compression [29,30]. In addition to damaged discs, other disorders, such as radial nerve entrapment, radiculopathy, and cervical facet syndrome produce neck pain.
When symptoms are aggregated, such as “pain and numbness into the thumb and index finger,” the dynamic changes. This may represent a subset of patients with just neck pain, i.e., of all patients with neck pain, not all have “pain and numbness, and pins and needles into the thumb and index finger.” This can be seen in radial nerve entrapment, thoracic outlet syndrome, C5-6 radiculopathy, C5-6 herniated disc, etc.
Symptoms of thumb and index pain and numbness:
- In right thumb - Numb
- In right thumb - Pins and Needles
- In right thumb - Constant Pain
- In right index finger - Numb
- In right index finger- Pins and Needles
- In right index finger - Constant Pain
These symptoms are compatible with a radial nerve entrapment, C5-6, and or C4-5 damage disc and associated radiculopathy, and elements of thoracic outlet syndrome, and overlaps with median nerve entrapment. Refer to the small example presented in (Figure 2) and (Table 2), in which the example patient had constant pain in the thumb and index finger which also was also numb and had pins and needles. DRM shows that 24 patients with some or all of these symptoms, when aggregated, had an abnormal provocative discogram at C3-C4 58.3% of the time, an abnormal provocative discogram at C4-C5 62.9% of the time, and an abnormal provocative discogram at C5-C6 51.8 % of the time. However, in 32 patients who had an MRI of the neck for these same set of symptoms, only 28.1% had a moderately or severely abnormal MRI, only 14.1% had an abnormal X-ray, and 33.3% had an abnormal 3D-CT. Additionally, 100% of the 12 patients with symptoms of radial nerve entrapment had an abnormal radial nerve block, and the root blocks from C4-C7 had positive results which ranged from 73-88%. From these data, a physician can determine which test will be most productive in confirming his or her diagnosis and will quickly recognize the rank order of positive testing as an aid in establishing a diagnosis.
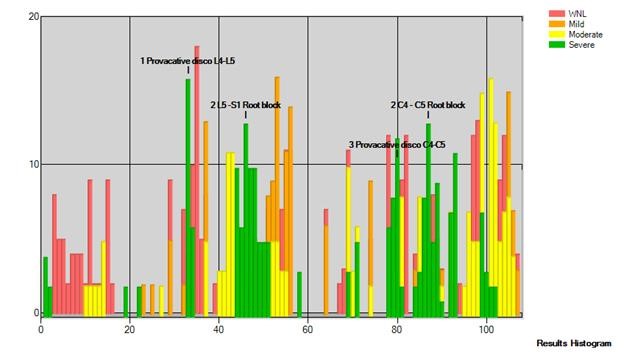
Figure 2: Pain and numbness into the thumb and index finger.
Table 2: For 6 Symptoms of thumb and index finger numbness, pain and pins and needles.

Discussion
The DRM serves as the benchmark against which symptoms of an individual patient can be compared. DRM is a stable and statistically valid tool that can evaluate any new patients’ Diagnostic Paradigm questionnaire and the specific answers they have compared to the large data base of medical test results. This resulting individual test evaluation can offer a numerical count of the patient’s potential test results and select the medical test most likely to be abnormal based on the highest frequency of this test. The rank ordering of medical test results declines based on frequency of abnormal results. This can be used to predict which test is most likely to be abnormal for which symptom.
In a practical clinical application, symptoms of an individual patient can be compared to the DRM’s data point system. Then, abnormal medical tests results can be predicted by comparing individual symptoms against the specified symptoms for DRM analysis. Individuals from a clinical setting can have their medical symptoms compared against the expected outcome of abnormal medical testing based on the data analysis by DRM. The results of the analysis will show that a predicted medical test will be abnormal for a certain symptom or grouping of symptoms. DRM has the ability to accumulate various symptoms, typically found in most disorders, to give overall expected medical test results for that constellation of symptoms. From this research, the percentage chance of a test being abnormal in any given patient can be predicted from the Bayesian Medical Accumulator. As an example, a typical report would say:
“In a compilation of 634 patients, from the Large Ordered Bayesian State Application (LOBSA), who had the same symptoms as the patient, 79% of them had abnormal finding on the provocative discogram, 54% had positive root blocks at C4-5, 51% had positive facet blocks at C4-7, 4 % had abnormal EMG/Nerve conduction velocity testing, 31% had abnormal CT, 28% had abnormal MRI, and 2% had abnormal X-rays.” This list of expected results will allow a physician or insurance carrier to determine, in a rank ordered fashion, the most productive test results which would be anticipated, through the least likely. More importantly, any test not listed on the expected testing list could be assumed to not have ever been ordered for a patient with the same symptoms as the example patient and, therefore, be totally unproductive.
What was immediately evident from these data is the value of physiological testing compared to anatomical tests when evaluating a patient with chronic pain. Anatomical tests, such as MRI, CT, and static X-rays, had a low percentage of abnormalities, because they merely take pictures. Physiological tests, such as stellate ganglion blocks, lumbar sympathetic blocks, provocative discogram, root blocks, peripheral nerve blocks, and facet blocks, had much higher positive findings, because they physiologically do something to the body, and the response is recorded [31]. Since pain is a physiological condition, a physician cannot take a picture of pain. Physiological testing is designed to administer a test, to see if it modifies, increases, or reduces, the pain for a patient. Anatomical tests do not do that.
The importance of obtaining abnormal test results rests with the ability to provide care for a patient. Clearly, abnormal testing produces an “actionable” event, i.e., something which a physician can address and correct if possible. By providing a physician with a list of what would be expected to be the most abnormal tests, rank ordered down to the least likely to be abnormal gives a physician a check list of tests to order, which would be the most likely to provide an opportunity for intervention, and treatment. Unnecessary testing or non-productive testing would be reduced or eliminated. Moreover, it helps a physician recognize a diagnosis which may have been overlooked and consider it in the differential diagnosis. The net results will be improved patient care, reduced treatment time and greatly reduced medical costs.
More information regarding this Article visit: OAJBGSR

No comments:
Post a Comment