Tuberculosis of the Breast with Erythema Nodosum: A Case Report by Richmond Ronald Gomes in Open Access Journal of Biogeneric Science and Research (OAJBGSR)
Abstract
There have been an increasing number of tuberculosis cases worldwide, but tuberculosis of the breast remains rare. In rare cases, this is seen with a cutaneous manifestation of erythema nodosum. We report the case of a 33-year-old woman with tuberculosis of the left breast accompanied by erythema nodosum on the anterior aspect of both lower legs and dorsum of feet. Due to her poor clinical response to conventional therapy, and the histopathological findings of fine needle aspiration cytology with epitheloid granuloma with caseation, there were strong indications of tuberculosis. She received anti tuberculous therapy for 6 months. During her follow-up examination after 6 months, no evidence of either residual or recurrent disease was present. Histopathological features and a high index of clinical suspicion is necessary to confirm a diagnosis of tuberculosis of the breast. Anti-tuberculous therapy (ATT) with or without simple surgical intervention is the core treatment.
Keywords: Tuberculosis, erythema nodosum, caseation, granuloma, anti tuberculous therapy.
Introduction
Tuberculosis (TB) is one of the leading infectious diseases worldwide. Extra pulmonary TB involving the breast is extremely rare. It often mimics breast carcinoma and pyogenic breast abscess clinically and radiologically, may both co-exist. Vulnerability to breast TB is increased in women who are young, married, multiparous and who breast-feed [1]. Histopathological examination using fine needle aspiration cytology (FNAC) may reveal caseating epitheloid cell granulomas and acid-fast bacilli (AFB). Although the presence of an acid-fast stain or culture is essential to confirm diagnosis, it does not give a positive result in most patients [2,3]. Molecular detection of Mycobacterium tuberculosis by polymerase chain reaction can be particularly useful in the validation of a diagnosis of tuberculosis in clinical settings where the diagnosis is uncertain [3,4]. Diagnosis is usually based on high index of suspicion, findings of granulomatous lesion with Langhans’ giant cells, tuberculosis culture and response to antitubercular therapy (ATT). We report a case of TB of the breast associated with a cutaneous manifestation of erythema nodosum.
Case Report
A 33-year-old married, recently detected diabetic( on metformin),HIV negative housewife presented at medicine outpatient, Ad-dinWomens Medical College & Hospital, Dhaka with fever, painful swelling over both shin and dorsum of the feet, bilateral knee and ankle pain for 8 days. She also gave history of gradually growing painful discharging lump over her left breast for last 1 month with on and off undocumented low grade fever. For the last 8 days fever became high grade, intermittent (maximum recorded 1030F) associated with chills and rigor and subsided temporarily after taking anti pyretic. She did not have any personal medical history of TB or diabetes mellitus. She also neither had family history of breast cancer nor had any contact history with a patient with active tuberculosis. She also denied any cough, weight loss, night sweat, anorexia, bloody diarrhea. She was immunized as per EPI schedule. With these complaints she visited a local physician and got 7 days 2nd generation oral cephalosporin without any improvement. She had a three-year-old child.
Upon admission she had a body temperature of 102 °F, blood pressure of 126/68mmHg, a pulse rate of 89/minute, and a respiratory rate of 19/minute. On physical examination, there was a firm, erythematous, mass of 5 × 6 cm with brownish discharge over the upper outer quadrant of her left breast accompanied by retraction of adjacent skin. Mass was not fixed to underlying structure or overlying skin. Nipple, areola was normal. There was also a firm, non-tender mobile lymph node over left medial axilla. Dark reddish plaque skin lesions were found over both lower legs and the dorsal aspect of her feet. Both ankle and knee joints were also red, swollen. There was also painful restriction of both active and passive movement in these joints. No other jointsor axial skeleton was involved. Her blood test results showed the following: Hb% 9.3 gm/dl, MCV- 81, MCH 29,white blood cells at 15.20 × 103/μL, neutrophils at 77.3%, lymphocytes at 12.7%, platelets at 418 × 103/μL, C-reactive protein at 86.8 mg/dL (normal range ≤ 5), and an erythrocyte sedimentation rate (ESR) during the first hour of 70mm/hour (normal ≤ 12).Peripheral blood film revealed normocytic normochromic anemia with neutrophilic leukocytosis. Her blood culture revealed no growth, while her chest radiography was unremarkable. MT was positive with induration 14 mm after 72 hours.
ALT 29 U/L, serum calcium 8,4 mg/dl, random blood sugar was 13.8 mmol/L. An ultrasonography of our patient's left breast showed a lump measuring about 5 × 5 cm, which was conglomerated, with an irregular margin with hypoechoic heterogeneous echogenicity, and with a left axillary lymph node. A core needle aspiration biopsy of her left breast was also performed. Under the microscope, this section of her left breast showed chronic mastitis mixed with granulation tissue and numerous foreign body giant cellsbut with no evidence of malignancy (Figure 1).Background consisted of necrotic material and fibrinous exudate. A culture of the wound tissues failed to grow any organisms. Stains for AFB were negative. Discharge for GeneXpert TB was not sent due to come unavoidable logistic support. A dermatologist was consulted regarding the dark reddish plaque skin lesions and treated conservatively with NSAIDs.
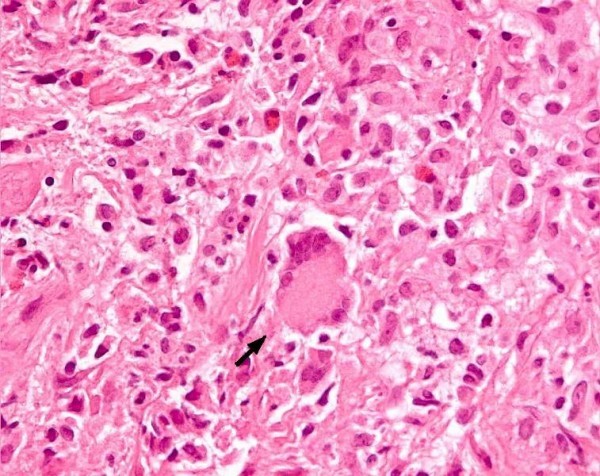
Figure 1: Hematoxylin and eosin stain of our patients breast tissue, showing giant cell(arrow) and Inflammatory cells.
Our final diagnosis tubercular mastitis was relied on clinical suspicion, histopathological tissue findings and failure to respond to conventional antibiotic therapy. She was put on a 6-month course of anti-tubercular therapy with a 2 month intensive phase of rifampicin, isoniazid, ethambutol, and pyrazinamide without steroid followed by a consolidation phase of rifampicin and isoniazid for another 4 months. After undergoing four months of anti-tuberculous treatment, her left breast mass and axillary node was gradually reduced. Although acid-fast stain showed no tubercle bacilli, her anti-tuberculous therapy was continued. Her left breast mass gradually became smaller and then regressed. She was treated for6 months without any further complication. She was regularly followed up for another 6 months and no evidence of the recurrence of her disease was noted Figures 2 & 3.

Figure 2: Healed ulcer with sinuses after 2 months of ATT therapy.

Figure 3: After 6 months of completion of AT therapy.
Discussion
Tuberculosis remains one of the leading causes of death from infectious diseases worldwide. Despite the fact that it can affect any organ or site of the body, the breasts, skeletal muscles and spleen are the most resistant to TB [5,6].Tuberculosis comprises approximately 0.025% to 0.1% of all surgically treated diseases of the breast, but this ratio is higher in underdeveloped countries [7]. The first description of mammary tuberculosis was given by Sir Astley Cooper in 1829 [5]. He described TB mastitis as “scrofulous swelling” in the bosom of young women. Although breast TB is primarily considered a disease of the developing world, a steady increase in the incidence of the disease has also been seen in developed countries. This is probably because of the migration of the infected population from endemic zones, and an increasing number of patients who are immune compromised [8]. Tuberculous mastitis is more commonly seen in females of reproductive age group, however, especially during the lactation period, when they are more susceptible since the lactating breast is more vascular and predisposed to trauma [4,5]. Both breasts are reported to be involved with equal frequency. Bilateral disease is rare, occurring in 3% of patients [5].
The duration of symptoms varies from a few months to several years, but in most instances, it is less than a year. Constitutional symptoms such as fever, weight loss, night sweats, or a failing of general health are infrequently encountered [2] and is present is less than 20% of cases. Our patient presented only a month history of breast lump without much constitutional symptoms. Its clinical manifestations are variable. Patients usually have a positive tuberculin skin test [9] so as our patient had. The common presentation of breast TB is a lump in the breast with or without ulceration, may associate with the sinus. Other presentations are diffuse nodularity and multiple sinuses. Multiple lumps are less common. Pain in the lump is present more frequently in breast TB cases than in breast carcinomas but our patient had painful breast lump. The involvement of the nipple and the areola is rare in TB. Fixation of the skin, which resembles a neoplastic lesion, may also be present but nipple discharge is uncommon. Associated axillary lymphadenopathy is found in some patients [1,3,10] as our patient had. Other uncommon presentations include; a typical undermined tuberculosis ulcer, purulent discharge from the nipple or with a fluctuant swelling which, if inadvertently incised, produces a discharging ulcer [5,11]. Both breasts can be affected equally but bilateral involvement is very uncommon. Although the upper outer quadrant seems to be the most frequently involved site due to its proximity to the axillary nodes, any area of the breast can be affected9. Lung lesions (active or healed) on radiographic examination are rare now. Mammography is of limited use since the findings are often indistinguishable from a malignancy [11] and young patients have highly dense breast tissue. Co-existing tuberculosis and carcinoma of the breast was reported by Alzaraa et al. [12].
Tuberculosis of the breast is mainly classified according to its primary and secondary forms. Although it was initially believed that as much as 60% of breast tuberculosis was primary, it is now accepted that mammary tuberculosis is almost invariably secondary to a lesion elsewhere in the body. Primary infection of the breast however, through abrasions in the skin or through the duct openings on the nipple is a possibility. The most common mode of infection is thought to be retrograde lymphatic spread from the pulmonary focus through the para- tracheal and internal mammary lymph nodes. Hematogenous spread and direct extension from contiguous structures are other modes of infection [5].
Breast tuberculosis was originally classified by McKeon et al [13] into the following categories:
a) Acute miliary type – rare, due to blood borne infection in miliary tuberculosis;
b) Nodular type – the most common type, which presents as a localized lump with or without sinuses in one quadrant of the breast;
c) Disseminated type – involving the entire breast with multiple sinuses;
d) Sclerosing type – minimal caseation and extensive hyalinization of the stroma, shrinkage of the breast tissue with early skin retraction and late sinus formation; clinically this type is indistinguishable from carcinoma; and (e) tuberculous mastitis obliterans – a rare form due to intra ductal infection with fibrosis and obliteration of the ductal system; sinus formation is infrequent [3,5,13]. Mantoux testing does not offer definitive diagnosis, but confirms exposure of the patient to tubercle bacilli.
Radiological imaging modalities like mammography and ultrasonography are unreliable in distinguishing breast TB from breast carcinoma. Similarly, computed tomography (CT) scan and MRI do not give a conclusive diagnosis without histopathological confirmation. CT scan is useful in differentiating between the primary and secondary forms. It is also helpful in evaluating the relationship between deeply located lesions with the chest wall and pleura and in detecting parenchymal lesions of the lung. As such it provides valuable guides to surgery and in defining the extent of the disease, including the involvement of the chest wall [10,14]. The demonstration of acid fast bacilli (AFB) from the lesions is usually difficult [15]. In tuberculosis mastitis, AFB are identified only in 12% of the patients. Our patient also did not show any AFB in the lesion. Therefore, clinical suspicion and demonstration of caseating granulomas with Langhans’ giant cells from the breast tissue and involved lymph nodes may be sufficient for the diagnosis. In tuberculosis-endemic countries, the finding of granuloma in FNAC warrants empirical treatment for tuberculosis even in the absence of positive AFB and without culture results [15,16].
Detailed histological evaluation is, however, mandatory to rule out a co-existing carcinoma. Core needle aspiration biopsy from our patients left breast revealed caseation, epitheloid giant cells without any evidence of malignancy. FNAC is very useful and it is a promising technique in expert hands16. A biopsy is mandatory for confirmation of diagnosis. Anti-tuberculous chemotherapy is still the main treatment for breast TB, and no specific guidelines are available for this kind of treatment. The disease should be treated as any other form of extrapulmonary TB. Anti-tuberculosis therapy comprises rifampicin, isoniazid, pyrazinamide and ethambutol for the initial two months, which is then followed by rifampicin and isoniazid for another four months. The extension of anti-tuberculosis therapy from 12 to 18 months is required in patients with slow clinical response, and complete resolution is obtained in most patients. Our patient showed response in 6 months so further extension of therapy was not given. FNAC should be repeated to confirm that the residual mass is fibrotic. In refractory cases that lead to breast destruction, a simple mastectomy may be performed [1,3,9,10]. Radical mastectomy is best avoided unless there is a co-existing malignancy [5,11]. The duration of follow-up after therapy is variable. In a study by Shinde all patients were followed up for a minimum of two years to determine that they were free of the disease after therapy1.After complete ATT, residual lumps localized to a quadrant should be excised via segmental or sector mastectomy. Aspiration or surgical drainage may be required in some cases.
The cutaneous involvement of TB is rare. Underlying systemic involvement of TB is often seen in cutaneous TB, especially in children. Cutaneous TB is classified as true TB or tuberculids. True cutaneous TB is composed of tuberculous chancre, miliary TB, lupus vulgaris, scrofuloderma, TB verrucosa cutis, tuberculous metastatic abscess and orificial TB. Tuberculids are delayed sensitivity reactions to M. tuberculosis in patients with a strong immune response. Tuberculids include lichen scrofulosorum and papulonecrotictuberculid. Facultative tuberculids consist of erythema induratum and erythema nodosum. Erythema induratum is a recurrent, painful subcutaneous nodule usually on the posterior aspect of the leg. Biopsy shows lobular panniculitis with vasculitis and granulomatous inflammation. Eythemanodosum is a painful subcutaneous nodule, mostly found on the anterior aspect of the leg. Biopsy shows septalpanniculitis with an absence of vasculitis and usually without granuloma. Erythema nodosum often occurs in association with a granulomatous disease, including sarcoidosis, TB and granulomatous colitis. TB remains an important cause of erythema nodosum in endemic countries [17-19].
Conclusion
In endemic TB regions, a painful breast mass with cutaneous manifestation of erythema nodosum is clinically relevant to determine a diagnosis of breast TB. To conclude, diagnosis of tuberculous mastitis is usually based on high index of suspicion, finding of granulomatous lesion with Langhans’ giant cells and response to ATT. FNAC and biopsy may also be inconclusive. AFB is not seen in most cases. Prompt diagnosis and adequate treatment can avoid unnecessary operation in these patients.
To know more about our Journal click on https://biogenericpublishers.com/
Open Access Journal of Biogeneric Science and Research (OAJBGSR)
No comments:
Post a Comment